|
Gen Measles
Stories to Help Us Understand
(These stories are written
in conversational style)
 General Measles
General Measles
(How the immune system handles an invader)
Script
Version click arrow
Audio Version
(Wav)
(MP3)
(Dr. Thomas O'Bryan)
General
Measles
(How
the immune system handles an invader)
Let's suppose you get a measles
shot. The brain recognizes that there has been an "invasion" by an
enemy. So it tells the immune system to appoint "General Measles" to
specifically go after the Enemy.
General Measles builds an
assembly line to manufacture "bullets" which are actually special "tags" with a "key"
mechanism on them. He makes the "key" to fit exactly and ONLY in
the measles molecule. Then he jumps in his Humvee, sticks his head out
the window and zooms around the body shooting his "tags" (antibodies) in
all the measles germs he finds. The tags mark the measles cells for
death. Other body cells see the tags and know to attack and kill the
measles germs.
When General Measles can't find
any more measles to shoot he turns off his assembly line, but for the rest
of his life he stays vigilant, searching ONLY for measles. If he ever
finds measles, he flips the switch, gets his assembly line
running, and goes back on active duty.
That is how our immune system
works. When we test for antibodies we look for the
"tags" that General Measles, General Casein, General Mumps, General Gliadin or
General Gluteomorphin, etc. use to "mark out" their particular
assigned enemy for death. Each
antibody is made to fit like a key in a lock ONLY in the specific
"enemy" that it was designed to tag.
But somehow this process is
going wrong. Sometimes the antibody "keys" stick in "locks"
or spaces where
they should not fit. (This is called "cross reacting. See more
on cross reactions in separate links on this website.)
This
literally nails "condemned" signs on our tissues and organs.
Special killer cells are attracted by the "tags/antibodies" like
a demolition crew looking for which house on the street to destroy.
When the antibodies stick in the tissues by mistake the killer cells then
mistakenly destroy our body tissues instead of just the enemy the were
intended to target.
This is "autoimmune disease".
 Close:
General Measles
Close:
General Measles
 The Five Branches of the
The Five Branches of the
Armed Forces
(and how they spot their man)
(Explains IgA, IgD, IgE, IgG, IgM)
Script
Version click arrow
Audio Version by
Dr. Thomas O'Bryan
(Wav)
(MP3)
The
Five
Branches of the Armed Forces
(and how
they spot their man)
(Explains IgA, IgD, IgE, IgG, IgM)
When our military looks for
evidence of action within their ranks, they are more likely to locate the
action and enemy if they check all branches of the armed forces (Army, Navy,
Air Force, Coast Guard, etc). Similarly, it is wise to check several
branches of our immune system/security system to find evidence of immune
activity against an enemy.
 What is "evidence of immune activity"?
What is "evidence of immune activity"?
What is evidence of immune
activity?
Symptoms may be evidence of
immune activity against a substance. However symptoms may not always
be evident, and they may be caused by more than one reason.
Therefore more specific proof of immune response is helpful, but symptoms,
if they are present, should be taken seriously
The immune system produces
antibodies to stick to or "tag" and identify an "enemy". Then "soldiers"
or killer cells see the "tag" and surround and
destroy the enemy. The antibodies can be observed and measured so it is common
to look for them and also for enzymes or "workers" that both may be involved
in immune reactions. These antibodies, enzymes and other
chemicals are found in body fluids or secretions like blood, stool, or
saliva.
 Close:
What is "evidence of immune activity"?
Close:
What is "evidence of immune activity"?
 Explain the branches of the immune system please. Explain the branches of the immune system please.
Explain the branches of the
immune system please.
Similarly to the above example of the
armed forces, when immune reaction to a food or substance is suspected
we look for the antibodies, enzymes or other reactions to that substance as
proof of immune activity. We are most likely to find these
antibodies/enzymes if we check several branches of our immune system. We
actually have
2 immune systems, the "innate" and the
"adaptive/acquired", and several branches of
those
2 systems. There are 5 branches of
the "acquired" immune system called
immunoglobulins.
IgA
- present in mucous membranes -
Definition
IgD -
a poorly understood immunoglobulin
-
Definition
IgE
- immediate allergic
histamine reaction -
Definition
IgG
- the most common immunoglobulin
-
Definition
IgM
- indicates present exposure -
Definition
For example, to test for
antigliadin antibodies (AGA) some testing labs check only the IgA
branch. Others check IgA and IgG, and others check IgA, IgG, and IgM.
Hence the individual tests are labeled,
AGA-IgA,
AGA - IgG,
and
AGA-IgM.
Why do labs vary in the
tests they run?
Opinions vary re the importance
of these antibodies mainly because AGA antibodies are often present
without visible villi (celiac) damage.
-
Other researchers argue that
damage may not always be to villi, but to other body areas instead,
and/or in some patients with genetic villi damage susceptibility.
Even then in patients susceptible also to villi damage, the damage
may not be advanced enough to be visible upon examination if villi damage
appears only in late stages for that patient. These
researchers argue that presence of AGA, AGA-tTG, or gluteomorphin antibodies
or other reactions by white blood cells (the ALCAT method) is ample proof
that the body is "fighting" gluten/wheat or other tested substances. They
recommend
treatment, i.e., avoidance of the substance such as gluten/gliadin,
milk or other tested substances. They also recommend protocols to heal
"leaky gut syndrome", a common cause for food intolerances.
 Close:
Explain the branches of the immune system. Close:
Explain the branches of the immune system.
 Close:
The Five Branches of the Armed Forces
Close:
The Five Branches of the Armed Forces
 Major Attack in Yemen!
Major Attack in Yemen!
(An immune system on high alert)
Script
Version click arrow
Audio Version by (Dr. Thomas
O'Bryan)
(Wav)
(MP3)
Major Attack in Yemen
(An immune system on high
alert)
Remember when the USS Cole
was attacked by in the harbor of Yemen? Terrorists loaded a
powerboat with explosives and crashed into the side of the ship. This was
a serious breach of United States security.
Question?
What happened to every US
Marine base around the world the day of the USS Cole attack?
Answer:
Even though the attack was
only in Yemen, it was such a severe breach of security that every Marine
base around the world went on high alert.
Is is postulated that a
similar phenomena may sometimes take place in our bodies. For
instance, bacterial or yeast infections or reactions to other foods like milk may be
so severe that the entire immune system stays up in arms. When the body
is under serious siege somewhere else, General Gliadin or General Casein may
be confused and continue to fire antibodies gliadin, casein or
other foods are no longer present. Those antibodies may
still cross react with tissues and initiate harmful inflammation and damage
to the body.
Lesson: In order to calm
overactive immune system responses, it is
important to find and treat the triggers. There may be several
triggers that could include gluten/gliadin, milk, yeast and fungal
infections fueled by dietary sugars and starches, other bacterial
infections, viruses, molds, other environmental and dietary toxins, and
toxic loads of heavy metals.
Therefore removal of gluten,
milk or other foods may be large pieces in the puzzle, but not be the only
pieces. Other "insults" to the body terrain may
create such serious immune response that the entire system runs on high
alert creating continued harm and havoc even after offending substances are
removed.
Removal of part of the
source is like carrying out only half the garbage. The kitchen still
stinks! You don't bring back the garbage you removed. You look
for the rest of the mess(es) and remove or treat them also.
Unfortunately, once the gut
is upset and out of balance, it may no longer to be able to digest many
foods efficiently, giving rise to multiple secondary food intolerances
hindering the natural ability to digest food such as eggs and (unprocessed)
milk that have historically nourished healthy populations for centuries.
Finally, farming methods, food
processing, additives, toxic exposures, unhealthy processed fats, emotional stress and increased physical separation from the
natural environment are all changes that parallel the rise of digestive/ degenerative/autoimmune
disorders?

Close :
Major Attack in Yemen!
 The Gatekeeper The Gatekeeper
The Zonulin Story
Script
Version click arrow
The Gatekeeper
The Zonulin Story
The following excerpt is
reprinted with permission from
Wheat Free Worry
Free:
The Art of Happy, Healthy Gluten Free Living
by
Danna Korn
Reprinted
with permission
Courtesy
of Danna Korn
Click to
download Adobe version
~~
Wheat and Gluten
May Be in Your
Future
(Contributions by Michelle Maria Pietzak, M.D.
and Alessio Fasano, M.D.)
“Every oak tree started out as a couple of
nuts who decided to stand their ground.”
Anonymous
In the last
several years, researchers around the world have focused on potential
treatments for wheat sensitive, gluten intolerance, and celiac disease.
Specific research on celiac diseases has attempted to understand the
mechanism by which gluten causes the presentation of this disease. In the
past few years, some exiting new discoveries have been made in this area
that may have equally important impacts on other conditions as well, such as
diabetes and multiple sclerosis. Recently, scientists at the University of
Maryland who were looking for the key to unlock some of the most baffling
mysteries about celiac disease shouted a very loud, “Eureka” followed by an
equally loud, “Open sesame!”
Zealots for
Zonulin
“Zonulin” may sound like a character from a science fiction movie, but it’s
actually a protein made by the human body, and may represent an important
piece of the puzzle in the development of autoimmune diseases, including
celiac disease.
The small intestine contains billions of cells that are packed so tightly
together that they act as a barrier against toxins, viruses, bacteria, and
other foreign invaders, protecting the body’s tissues. Between these cells
are the “tight junctions” (also referred to as the zonula occludens).
Researchers wondered how gluten, a relative large molecule, was getting
through the tightly packed cellular barrier and into the immune system where
it caused an autoimmune response. The answer, they discovered recently, is
that exposing the small intestine of the celiac patient to gluten causes an
increase in the production of the protein zonulin. Zonulin decreases the
resistance of the small intestinal barrier by opening the tight junctions,
which can then open the spaces between cells, allowing some substances to
pass through. In other words, zonulin acts as the gatekeeper for the body’s
tissues. People with celiac disease and some other disorders have higher
levels of zonulin, which, in essence, means that gates are “stuck open,”
allowing gluten and other harmful substances to pass through.
An
Unexpected Discovery
The story of the discovery of zonulin is an interesting and unique example
of how scientists can learn from microorganisms (for example, bacteria).
Researchers at the Center for Vaccine Development at the University of
Maryland were trying to develop a vaccine for the cholera bacterium (cholera
is one of the leading causes of death in children worldwide, and it causes a
profuse, watery diarrhea). The researchers discovered that cholera causes
diarrhea by secreting a toxin called Zot (zonula occludens toxin), which can
open the tight junctions (zonula occludens), thereby contributing to the
severe, life-threatening diarrhea. Being keen scientists, they realized
that these smart bacteria were likely mimicking a natural process in the
human body. Using the latest techniques in molecular biology, they
identified zonulin, a human protein that binds to the same receptor as Zot
and performs similar actions.
The researchers found that zonulin was elevated in the tissue of subjects
with many different diseases, such as celiac disease, type 1 diabetes
(insulin-dependent or childhood diabetes, also a autoimmune disorder), and
multiple sclerosis. They hypothesized that zonulin opens the tight
junctions in these individuals, and allows molecules to pass across the
intestinal barrier that normally would not pass through.
In a person with celiac disease, production of zonulin increases in response
to eating gluten. This leads to more open tight junctions between the
intestinal epithelial cells, allowing the passage of toxic portions of
gluten (which are normally too large to pass through). These toxic portions
then interact with our friend tTG (tissue transglutaminase; see section on
antibody testing for celiac disease), which changes the gluten fraction to a
form that can interact with the immune system’s lymphocytes (specialized
white blood cells).
These interactions lead to the production of cytokines, chemicals that
attract more lymphocytes to the affected area. The lymphocytes then attack
the small intestine epithelium, leading to blunted or flat villi. Some
lymphocytes will also be stimulated to produce specialized antibodies, the
antigliadin, antiendomysial, and anti-tissue transglutaminase antibodies.
These antibodies do not damage the intestine, but can be used as markers for
celiac disease when they are found in the blood in elevated
concentrations.
Zonulin and
the Blood-Brain Barrier
Researchers
at the University of Maryland were on a roll. Having discovered the
importance of zonulin in opening the spaces between the cells that serves as
a barrier in the small intestine, they turned their attention to the
blood-brain barrier. The blood-brain barrier, like the barrier created by
tightly packed cells in the small intestine, is a collection of tightly
packed endothelial cells that line the blood vessels of the brain and
prevent some substances in the blood from entering, while allowing others to
pass through. Until now, scientists knew very little about why some
molecules were allowed to pass through and other were not. The researchers
hypothesized that zonulin could play a similar role in the blood-brain
barrier to the one it play in the intestinal epithelial barrier, by opening
the tight junctions or gates between the cells in the blood vessels of the
brain.
Their theories have been substantiated; they have now verified that the
receptor that binds both zonulin and Zot exists in the brain. This
discovery may lead to novel treatments of diseases in which there is
blood-brain barrier dysfunction, such as multiple sclerosis, brain tumors,
and HIV infection.
The fact that zonulin receptors exist in the brain, and that zonulin is
increased in the tissues of patients with celiac disease, may provide an
explanation for some of the neurological symptoms of the disease. Also, the
possibility that doctors may be able to deliver new types of medications
(linked to Zot or zonulin) across the blood-brain barrier could open the
doors to a whole new world of treatment options for many neurological
diseases.
Technical info here,
here, and
here
 Close:
The Gatekeeper
Close:
The Gatekeeper
 A Life of it's Own
A Life of it's Own
or
Mousetraps on a Football Field
(Explains cascade reactions)
Script Version click arrow
Audio Version by
Dr. Thomas O'Bryan
(Wav)
(MP3)
A
Life of
it's Own,
or
Mousetraps on a Football
Field
(Explains cascade reactions)
Question? Why does it take so little gluten or other poorly
tolerated substances to set off a strong reaction?
How many mousetraps are
needed to cover a football field?
Final calculation!
976,000!!
Imagine 976,000 mousetraps
all cocked with a ping pong ball, covering a football field. Now walk
along the side of the field and flick a ping pong ball onto the field.
It sets off the trap it hits, and now 2 ping pong balls pop
in the air. Then 4, 8, 16, 32, 64 and on and on. The
field takes on a life of it's own and likely long after the original ball that began
the cascade rolls into oblivion. The reaction continues
unmanned.
The behavior of a presensitized immune
system is somewhat similar to this rather amusing illustration - but without the fun!!
If we are presensitized to gluten or some other substance, immune system
cells are primed to react in a complex cascade fashion to even very small exposure.

Close:
A Life of it's Own
or Mousetraps on a Football Field
 Dominoes on a Football Field
Dominoes on a Football Field
or
(Why does just a small amount matter? and Why no symptoms or only delayed symptoms?)
Script
Version click arrow
Audio
Version (Wav) (MP3)
Dominoes on a Football Field
or
(Why does just a small amount matter? and Why no symptoms or only
delayed symptoms?)
It is helpful to envision a
football field covered with dominoes lined up on end in sequence. A
very tiny nudge on the first domino commences the tumble process.
However, due to the number of dominoes involved the reaction takes
significant time to complete.
Similarly, a small
amount of an offending substance ingested by a sensitive person, may
initiate an
incredibly complex reaction process that
may continue for days. Many reactions in the sequence may
affect areas of the body which lack nerve endings, and thus create silent
damage. It may be days before a domino "falls" so to speak that
produces pain or a noticeable symptom. This may hinder the patient's
ability to identify an offending substance ingested days
earlier.
 Close:
Dominoes on a Football Field
Close:
Dominoes on a Football Field
 The Strong Survive
The Strong Survive
(A reason why reactions to dietary "mistakes" may be stronger after healing takes place)
Script
Version click arrow
Audio Version (Wav) (MP3)
The Strong
Survive
(A
reason why reactions to dietary "mistakes" may become stronger after healing takes place)
When a patient is sensitized
to a substance and then removes exposure to the substance, most of the
affected cells' reactive activity may "go to sleep", and the
irritation/intolerance reactions are calmed. However, upon exposure to even
a very small amount of the offending substance, only the strongest cells may
"wake up" to react. The cells that "wake up" may the be the strongest
cells in the pack, and they reproduce more strong cells. This
phenomena predetermines that individual reactions after general removal of
the offending substance may be stronger than before general removal.
Moral of the story :
"Crumbs matter!"
 Close: The Strong Survive
Close: The Strong Survive
 A Garden Hose
A Garden Hose
and a Power Surge
(Brain Ischemia/Reperfusion Injury)
Script
Version click arrow
Audio Version
(Wav)
(MP3)
(Dr. Thomas O'Bryan)
A Garden Hose and a Power Surge
(Brain Ischemia/Reperfusion Injury)
1: Lijec Vjesn. 2006
Mar-April:128(3-4):87-95
[Pathophysiology
of ischaemia-reperfusion injury] [Article in Croatian]
Sirotkovic-Skerlev M,
Plestina S,
Bilic I,
Kovac Z.
Katedra za patofiziologiju Medicinskog fakulteta u Zagrebu.
Reperfusion of ischaemic tissue provides oxygen and substrates that are
necessary for tissue recovery and concurrently removes toxic metabolites.
However, reperfusion may induce various detrimental processes that may cause
further tissue damage. Such deterioration of tissue function after
reperfusion is defined as ischaemia-reperfusion injury. The consequences of
ischemia-reperfusion injury vary from reversible cell dysfunction to local
and remote tissue destruction, multiple organ failure and death. The
pathogenesis of ischaemia-reperfusion injury is complex and includes
excessive production of reactive oxygen species, activation of neutrophils,
activation of complement, involvement of cytokines and other inflammatory
mediators, vasoactive substances NO and endothelin. This review discusses
the pathophysiology of ischaemia-reperfusion injury, the mechanisms of
reactive oxygen species production, and the role of other factors in the
pathogenesis of such injury. Several approaches and procedures used in
pre-clinical and clinical studies in order to limit ischaemia-reperfusion
injury are also presented.
PMID: 16808098 [PubMed - in process]
A Power Surge
Ischemia - Reduction of
blood flow
Definition
Reperfusion - restoration of
blood flow
Definition
Since the link above is a
technical article, it is easier to also illustrate ischemia/reperfusion
injury in the following story.
The on/off phenomena of
ischemia-reperfusion injury may be compared somewhat to an electrical
brownout or blackout. When electrical power is cut off we unplug our
sensitive electrical appliances including computers, fax machines,
microwaves, etc., and/or provide surge protectors to minimize damage
to sensitive circuitry.
Consistent blood flow is
vital to every area of the body, but especially to organs and it is crucial
for the sensitive brain. (The brain lacks a reserve supply of cell
fuel called "organ reserve" that other organs possess to carry them through
momentary deprivation. See www.pubmed.gov for over 2000 discussions of
brain, ischemia and the phenomena of general ischemia-reperfusion injury).
Medicine is well aware of
damage incurred by off/on blood flow to tissue, and attempts to minimize
this damage is the subject of extensive study. Other examples of
ischemia-reperfusion injury to tissue include on/off blood flow during
heart attacks, heart surgery, or hypothermia. Injury occurs when when
blood flow returns to deprived tissue. The brain is particularly
sensitive to this type of damage.
How does
ischemia-reperfusion injury apply to individuals who are immune sensitive to
foods such as gluten or milk, yeasts, molds, and/or other
environmental substances?
The Garden Hose
A large blood vessel travels
up each side of the neck like a garden hose, carrying blood into the brain.
Once it reaches the brain it divides into smaller vessels to distribute
blood to various parts of the brain, like a sprinkler attachment on a garden
hose. In the garden hose example, if the sprinkler is set correctly,
every part of the lawn receives an adequate supply of moisture and all is
well. However, if the sprinkler is partially clogged, or
inappropriately set so parts of the lawn are not adequately watered, then
vegetation in those areas fail to thrive or die.
Research was performed of
patients known to be gluten sensitive but not yet treated with the gluten
free diet. These patients were subjected to SPECT scans (color images)
of the brain. Reduction of brain blood flow was
noted in an average of 4 areas per patient compared to normal blood flow in
healthy controls. SPECT scans were repeated after implementation of a
gluten free diet and normalization of blood flow was observed.
Reintroduction of gluten in the diet reproduced areas of reduced blood flow.
This mechanism is of grave
consequence to patients adhering to the gluten free diet or other
diets/treatments designed to remove substances known to induce immune
response and its consequent damage and inflammation.
If a sensitive patient
adheres to a strict diet or lifestyle which excludes offending substances,
research indicates that blood flow is not impaired by the immune induced
reactions and inflammation caused by these substances.
Occasional (off and on)
ingestion of immune reactive substances such gluten or milk in sensitive
individuals may recreate a number of adverse processes including
inflammation and temporarily reduced blood flow in various areas of the
body. Return to a gluten free diet again normalizes blood flow, but
not with risk of the damaging effects of ischemia/reperfusion injury.
This is a difficult state of
affairs. Lack of blood flow is not an acceptable state of affairs, but
accomplishing return of blood flow through exclusion of inflammatory
substances carries it's own inherent risks.
This principle illustrates
the rationale behind unwavering recommendations by specialists in the gluten
sensitive community to adhere strictly to the gluten free diet. The
relationship between ischemia-reperfusion injury and "cheating" on the
gluten free diet, such as occasional birthday cake, communion
wafer/loaf, an inappropriate brand of gluten containing soy sauce at a
restaurant, or the more prolonged gluten challenge for diagnostic purposes
is not widely understood in the gluten sensitive community.
Close: Click link at the TOP of story
A metal key
in a foam rubber lock?
(Discusses antibody cross reactions and possible relationship to dietary
fats)
Script Version
Audio Version (Wav) (MP3)
 Remember the Mousetrap Game?
(Explains the need for nutrient dense food)
Remember the Mousetrap Game?
(Explains the need for nutrient dense food)
Script
Version click arrow
Remember
the Mousetrap Game?
( Explains
the need for nutrient dense food)
Script
Version click arrow
Audio Version (Wav) (MP3)
"Mousetrap" is a children's
game in which a series of amusing contraptions are linked together to form a
"fantasy pathway" which a ball rolls over/ under/through. Each piece
added to the pathway allows the ball to activate the next piece until
finally the ball disengages a cage that falls and captures a "mouse".
Many adults today remember
this childhood game and are aware that even one missing piece in the pathway
causes the ball to roll off the course and be lost.
Similarly in our bodies,
thousands of chemical reactions take place every second, one after the
other. The steps in these pathways
need certain "pieces or ingredients" to accomplish each reaction. If
those ingredients are not available the reaction and successive reactions may not happen,
and
digestion, healing and many other processes are hindered.
Homocysteine is an example
of this phenomenon. Homocysteine is formed naturally in the body as an
amino acid, methionine, is broken down into energy. There are 8
successive steps or reactions needed to metabolize (break down) methionine,
and homocysteine is formed during one of these 8 reactions.
Several chemicals are needed to take homocysteine to the next step including
betain, folic acid and several B vitamins. If these ingredients are
not available, homocysteine pools in every body cell, more particularly in
some areas and organs than others. This pooled homocysteine is "gas on
the fire" when inflammation is present and is known in medical fields to
contribute at times to conditions such as sudden death by heart attack and
Alzheimer's Disease.
When the missing ingredients are provided for the next chemical reaction in
the metabolic succession, homocysteine is converted properly and the "bottleneck"
is relieved. This is easy, inexpensive and often quickly effective.
Moral of the story
If we consume poor quality
over processed "fuel" (food) or toxic substances that lack or actually
rob the supplies our body
needs for chemical processes, we may no longer feel hungry but our body
lacks the pieces it needs to complete chemical reactions required for
proper function.
Today much of our soil is
depleted and food grown on it may lack the "building blocks" needed to
supply these chemical reactions. Additionally
nutrients are diminished or chemically altered by food processing.
Furthermore, toxins require our bodies to work very hard in it's attempts to
remove them. This increases the demands for nutrients normally intended for
healthy function.
Close link:
Remember the Mousetrap Game?
 A Table with 100 Legs
A Table with 100 Legs
Why so much
illness in children and young people??
Or
Why
do some people enjoy "reasonable" health even when
their diet and lifestyle is poor.
Script
Version click arrow
A Table with 100 Legs
Or
Why so much
illness in children and young people?
Or
W hy
do some people enjoy "reasonable" health even when
their lifestyle is poor.
Script
Version click arrow
Picture a table with 100
legs. If a few are knocked out it's not usually a significant problem.
There are plenty left to keep the table sturdy and standing. Even if
it loses 80 legs it will probably be OK depending on how they are placed.
But if it loses 97 legs, now
there is a problem. A table normally needs 4 legs placed at each
corner and they need to be sturdy enough to support the table's weight.
Now there are no "extra" legs to compensate for the required fourth leg.
Similarly our bodies are
normally built with plenty of "backup building blocks" when the lifestyle and
diet are reasonably adequate and the body compensates for temporary hardship. Over the centuries diet and lifestyle
has rarely been perfect. However, prolonged abuse may
"knock out some of the table legs", and over the generations
each set of parents may pass a reduced heritage of prenatal health
and in toxic exposure and lifestyle habits. Eventually the
accumulated deficiencies become so extreme that there is reduced ability to
compensate. Subsequent generations of children are not born with the pieces or
building blocks they need to grow and function normally. A person who
functioned well previously may exhaust their body resources and general
wellbeing is compromised.
 Close link:
A Table with 100 Legs
Close link:
A Table with 100 Legs
|
For latest version of each
page on this website click "refresh" on your browser tool bar.
Last updated Jan. 12, 2011
Look up medical terms
here
Tests for The Gluten Syndrome
and other cross reactive food
reactivities,
toxins,
environmental allergies
and
 Tests specifically
Tests specifically
focused
on diagnosis
of
villi damaged
celiac
disease
(Thought
by some researchers to be
a
small
subtype of the gluten syndrome.)
~~~
Due to large page size,
the
Lab Charts
have
moved to a separate page.
The most sensitive and comprehensive tests are discussed on this page
and also
here and on
the expanded index page.
A black arrow  identifies a "show/hide"
link.
identifies a "show/hide"
link.
Click to open and close link.
There are several
perspectives of gluten syndrome testing, plus constant new developments.
It is unfair to expect any one professional to stay updated perfectly at all
times. Patients
have more time than their doctors to investigate their condition.
This helps them choose or change to qualified, open
minded professionals to whom they bring information for evaluation.
Humble, open minded professionals pay attention to well conducted research.
Prayer, diligence,
courage, and common sense balanced with openness and flexibility are
valuable attitudes in the search for guidance.
How does a lay person find
information and research?
 How does a lay person find information and research?
How does a lay person find information and research?
Readers are encouraged to
learn the various types of research articles,
and how to find and evaluate them.
Research resource links
www.pubmed.gov
www.pubmed.gov is a free
public medical research resource with
helpful tutorials.
To search PubMed for a
possible connection between a given condition and gluten, type "gluten", "gluten
intolerance", "celiac disease", "coeliac disease",
"gluten sensitivity" and (name of the disease) in the search bar.
Examples: CELIAC DISEASE AND DOWN'S SYNDROME or GLUTEN AND
HEADACHES.
Articles are listed with free
links to the full text, or a short summary called an abstract, and some
have no further information available. Sometimes a local library can
obtain articles upon request.
Note: Search engines
are not perfect. If a search comes up empty, try using other terms,
or combinations. Some words do not come up when they are known to be
in the database. Also a search may be empty because a research
article is not loaded into this database or research has not yet been
performed.
Links to online medical
dictionaries:
http://www.nlm.nih.gov/medlineplus/mplusdictionary.html
http://cancerweb.ncl.ac.uk/omd/
Celiac focused research
sites are found on the
Resources page of this website.
Research articles that
cover a wider scope of the gluten syndrome are found at the following
websites:
www.enterolab.com
www.immunoscienceslab.com
This website, bottom of
Medical Diagrams page and the
Lab Charts page under Neuroimmunology
Labs.
Understanding your tests - Helpful articles from
www.labtestsonline.org
 Close:
How can a lay person find information and research?
Close:
How can a lay person find information and research?
"Testing Viewpoints Checklist"
Note: Due to the high number
of expand/collapse links on this page it is recommended that the reader
close each link as each section is read to keep the page clean and make it easier to
relocate information.
 A.
A basic tutorial of test processes A.
A basic tutorial of test processes
A basic tutorial of test processes
 1. Is this test credible?
1. Is this test credible?
1. Is this test credible?
If
the test is unvalidated,
-
Why is it unvalidated?
Sometimes there are explainable reasons.
-
Who developed the test?
-
What motivators influenced the
work?
-
What track record/reputation does this
test maintain. Does it match patient experience when test results and clinical
results are compared?
The gluten syndrome community
has a home stool test available
www.enterolab.com, for which the
research is not published or validated at this time. However public
confidence has grown considerably in the test over the past 8 years.
It produces a high number of positives and in most cases the results match
patient experience. More on
this test on this page.
 Close link: a. Is this test credible?
Close link: a. Is this test credible?
 2. How accurately was this sample processed?
2. How accurately was this sample processed?
-
Was it performed correctly?
-
Were quality materials
used to process the test.? Sometimes this is a problem.
-
Was it read correctly?
Processing employees may be inexperienced.
-
Did the doctor interpret the
results in an accurate context or paradigm? (ex. celiac only or the wider
gluten syndrome perspective.)
 Close link: How accurately was this sample processed?
Close link: How accurately was this sample processed?
 3. What is the goal of the test or test panel?
3. What is the goal of the test or test panel?
3. What
is the goal of the test or test panel?
Contrasted examples of test
goals include:
-
Blood antibody test panels - Does the test check
for
IMMUNE RESPONSE (antibodies) to gluten related substances? (Ie., is the body
fighting gluten?). Why is this important? Some
researchers believe presence of antibodies alone is proof that
gluten should be avoided. They believe the antibodies can damage many
tissues of the body. Some of them may be
difficult to find. But the antibodies prove a immune reaction is present.
-
Villi biopsy - This test checks for damage to one specific body tissue only, the villi. Why is this important?
Celiac specialists use villi damage only to confirm immune reaction to
gluten and prescribe a gluten free diet. If gluten antibodies are are
present but there is no villi damage they ignore the antibodies. They do not count the very presence of
antibodies as proof that the immune system reacts to gluten nor the possibility that in many cases damage may occur
to other areas of the body
and NOT the villi.
 Close link: 3. What is the goal of the test or test
panel?
Close link: 3. What is the goal of the test or test
panel?
 4. What are the best test mediums, and why?
4. What are the best test mediums, and why?
4. What are the best test mediums, and why?
Blood, saliva,
white blood cells, stool, skin or villi biopsy, energy based testing are
mediums used for testing gluten reactions.
Celiac specialists use blood
tests, and villi or skin biopsy
only. They use blood antibodies because they show a reaction circulating in
the bloodstream.
Gluten syndrome specialists use
blood, stool*
and saliva. (Some alternative practitioners use energy based testing
such as bioenergetic testing.) They believe elevated antibodies in any
medium are conclusive proof of a reaction to gluten and they may show up in
stool or saliva earlier than in blood.
*Since
it is normal to have a few antibodies in stool to most foods we eat, the
reference ranges are adjusted to account for these normal levels.
Specific villi or skin damage is
considered proof by both celiac and gluten syndrome specialists to be caused
by gluten (sometimes milk in the case of villi damage) However gluten
syndrome specialists believe villi damage is only one of many places gluten
may target for damage. They also say that if other tissues but NOT the villi are damaged, that a
villi biopsy is useless. Skin biopsy is only performed if there is
visible damage (dermatitis herpetiformis).
As more literature is published
on saliva tests, more patients now turn to these tests due to low
cost, and easy collection. If their saliva tests are negative they may
move on to more detailed antibody tests or other mediums such as blood to check out more possibilities.
Since there are antibodies for which there are no tests, any negative test
must necessarily be inconclusive for diagnosis of the gluten syndrome.
 Close link: 4. What is the test medium, and why?
Close link: 4. What is the test medium, and why?
 5. What does this test measure or observe?
5. What does this test measure or observe?
5. What does this test
measure or observe?
Standard gluten related tests measure antibodies,
the tTG
enzymes, and villi or skin damage. However, 2 labs test the function of
other organs or tissues
www.enterolab.com
and Immunoscienceslab.com), looking for possible gluten related damage.
Other labs, ALCAT and ELISA/ACT Biotechnologies, each measure different white cell
reactions to gluten related substances. The ALCAT test is
controversial.
 Close link: 5. What does this test measure or
observe?
Close link: 5. What does this test measure or
observe?
 6. How sensitive, specific, or detailed is this
test/test panel?
6. How sensitive, specific, or detailed is this
test/test panel?
Sensitivity - Some tests are sure to find a
substance when it is present. Other tests may miss the item sometimes.
This trait is called "sensitivity". If a test runs 100
samples that all are actually positive, and it find the substance in 75 of
the samples (positive) then it is 75% sensitive.
Specificity - Some tests identify a
"specific substance" very well. The test may not always find the item
when it is present, but when it does find it, it only finds that item
without confusing it with something else. If a test runs 100 samples
that are all positive and correctly identifies the tested substance in 75
samples without confusing it with something else in the sample, then it is
75% specific.
Limitations - Some tests (
blood or saliva antibody tests) are
only accurate when the patient has eaten gluten for a period of weeks or
months before the test. The
www.enterolab.com
stool test can be used for several months after the patients goes GF because
they claim the antibodies hang around in the gut longer than the blood
stream. The ALCAT test does not require a gluten containing diet. the
ELISA/ACT Biotechnologies test requires one serving of gluten within the
past 6 months.
 Close link: 6. How sensitive, specific, or detailed is this test?
Close link: 6. How sensitive, specific, or detailed is this test?
 7. Does the test account for variations such as time of day, diet or other
factors?
7. Does the test account for variations such as time of day, diet or other
factors?
Examples:
-
Is only one
test/collection accurate, or do levels rise and fall at different times of
the day, necessitating a series of tests/collections repeated at intervals
in order to reflect these variations? Answer? Good
question!!!
Blood and saliva tests - Yes a
gluten diet is required for weeks or months prior to the test.
NOTE:
If the patient is already completely off glutenfor a number of weeks
depending on the person, experience indicates that
many patients are miserable if they go back in order to be tested, and it
has been downright harmful, even psychiatrically, for some.
Stool testing (www.enterolab.com)
claims that the test works for weeks or months after the gluten free diet is
begun, because the antibodies hang around in the gut that long. Call
the lab to ask.
 Close link:
7. Does the test regime account for variations such as time of day, current
diet or other lifestyle deviations?
Close link:
7. Does the test regime account for variations such as time of day, current
diet or other lifestyle deviations?

8.
How does this test's results match the experience
of the patient community?
 9. Do test results fit the individual's experience?
9. Do test results fit the individual's experience?
9. Do test results
match what the individual's own body tells him, taking into account the known
nature of the condition in question?
The patient's own body often is a reliable judge. However, in the case
of gluten there are some confounding factors to consider as a reaction or lack of it
is evaluated. These can be confusing at first.
1. Some serious gluten related reactions/conditions may be SYMPTOMLESS
for long periods of time sometimes due to delayed reactions or damaged,
silenced nerves.
2. The patient may have uncomfortable healing
Herxheimer's or retracing
reactions in which symptoms actually regress temporarily as healing takes
place, or other food intolerances and imbalances are still untreated, or
retracing (copies) of old health and emotional events occur.
(Retracing is a homeopathic concept.)
3. Sometimes a withdrawal effect may be experienced.
Gluteomorphins may exert an opiate like affect on the brain and removal of
them may produce temporary withdrawal.
Taking the above variations into account, what might the patient's own body
tell him regardless of test results? This may be highly significant. Many
patients and their doctors tend to believe negative tests even when the
patient's body clearly says that gluten is not OK. Others realize
negative tests are inconclusive and take
their body's message very seriously. They recognize that this field
with it's testing methods, is still in it's infancy.
 Close link: 9. Do test results match what the
individual patient's body tells him, taking into account the known nature of
the condition in question?
Close link: 9. Do test results match what the
individual patient's body tells him, taking into account the known nature of
the condition in question?
 10. What new research is anticipated?
10. What new research is anticipated?
10. What new research is anticipated?
What future options may become available as patients evaluate today's
choices?
A gluten related test protocol
is proposed that runs the most common gluten antibodies first and progresses
through the list of available known antibodies until a positive is reached
or all have been tested. This progressive test panel conserves total
cost and the patient need only submit specimens once.
Watch the home page of this
website for further information. This website has no financial
interest in any product or service mentioned here.
 Close link: 10. What new research is
anticipated?
Close link: 10. What new research is
anticipated?
 Close
link:
A.
A basic tutorial of test processes Close
link:
A.
A basic tutorial of test processes
 B. Understanding gluten syndrome tests and also the tTG (tissue
transglutaminase) test often used to specifically screen for celiac (villi ) damage
only.
B. Understanding gluten syndrome tests and also the tTG (tissue
transglutaminase) test often used to specifically screen for celiac (villi ) damage
only.
 1. What are the tests looking for?
1. What are the tests looking for?
What are the tests looking
for?
Tests look for evidence that
that the immune system has manufactured antibodies and/or an
enzyme to "tag" various pieces (peptides) of poorly digested gluten.
Please explain peptides and
antibodies?
-
During digestion gluten breaks
up into pieces called peptides, but it resists breaking up completely, which
is not good. The peptides are still too large. If the gut wall is in poor
shape, these pieces may slip through the wall before they are properly
broken down.
Here is a list of peptides that
form as gluten breaks up, and the corresponding antibodies the body makes to
"tag" them.
Gluteomorphins - pieces
of the gluten molecule. - Gluteomorphin Antibody
Gluten - Gluten
itself, the whole molecule, is tested by only a few labs.
Gliadin - a piece of
only wheat gluten - Antigliadin antibodies (AGA)
Hordein - a piece of
only barley gluten - Antihordein antibodies (not tested)
Secalin - a piece of
only rye gluten - Antisecalin antibodies (not tested)
Avenin - a piece of
only oat gluten - Antiavenin antibodies (not tested)
Example: Below is a fun
illustration of the wheat gluten molecule before it starts to break up.
Click the title for an explanation.

 The Gliadin Mouse in the Gluten House
(Click for details) The Gliadin Mouse in the Gluten House
(Click for details)
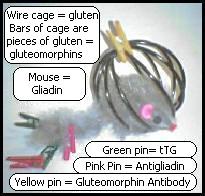
"The Gliadin Mouse in the Gluten House"
-
In this illustration, the
black wire "cage" represents
gluten, a large
complex protein molecule. When the bars of the "cage" begin to break
apart during digestion, "gluteomorphins"
and other glutenins are formed.
-
The green and yellow clothespins represent
different specific antibodies that the immune system makes to "tag" gluteomorphins, gliadins and other lesser known glutenins as if they
were foreign invaders. This marks
them for destruction. Each antibody is designed to tag only that
particular peptide (piece) but some researchers say they make mistakes and
also tag
body tissues that look a little bit like that peptide. This attracts killer cells to innocent
body tissues and creates inflammation and autoimmune disease.*
When the antibodies tag
innocent "look alike" tissues or similar foods, this is called "cellular
mimicry".
*Published
research observes that due to their structure, antigliadin, gluteomorphin, and casomorphin
(milk) antibodies bind or "cross react" with brain and nerve tissue and many
other organ and body tissues by cellular mimicry. This means
these antibodies are particularly dangerous. See Immunosciences Laboratories on the
Lab Charts page for references.
 Close:
The Gliadin Mouse in the Gluten House
Close:
The Gliadin Mouse in the Gluten House
Celiac specialists check
very few antibodies but rely mainly on tTG and villi biopsy for dx.
Gluten syndrome oriented specialists (there are few of them), test for
all the antibodies they can until they get a positive. They do not perform an
invasive biopsy unless there are other reasons to examine the gut because
they recognize that damage could be to many different locations, and only
occasionally the villi (1 in 100).
-
A few celiac specialists may
check antigliadin (AGA) antibodies, but most do not since they are confused when they get
positive gliadin antibodies but negative biopsy. Unfortunately instead of
questioning the biopsy as the only possible place of damage, they ignore
the positive antibody test, even though antibodies are proof in themselves
of an immune reaction.
-
Gluten Syndrome
specialists include gluteomorphin, gluten, wheat, and IgM antibodies
in
addition to the tTG and gliadin markers used by celiac specialists.
When they look for more antibodies, they find many more positive testing
patients. (One doctor,
Thomas O'Bryan, Chicago, tested all his patients,
350+, over a 3-4 year period and
77% of them were
positive for a gluten related antibody!!)
Celiac vs. gluten syndrome
specialists vary on their interpretation of antibody tests
Gluten syndrome specialists believe that
any positive gluten related antibody test proves that
the body is fighting gluten or wheat. They believe that the villi are not always
damaged, but that the
damage is often somewhere else
in the body. Therefore they use high antibodies, NOT villi biospy as a
diagnostic tool. They also pay attention to the patient's symptoms since
a few gluten syndrome patients may have antibodies for which there are no tests and
therefore may test negatively in even the most complete panels.
 Close: What are the tests looking for?
Close: What are the tests looking for?
 2. List of tests, their abbreviations and descriptions
2. List of tests, their abbreviations and descriptions
 ANTIBODY TESTS ANTIBODY TESTS
 a.
AGA - Antigliadin Antibodies
a.
AGA - Antigliadin Antibodies
a.
AGA - Antigliadin Antibodies
Antigliadin Antibodies
are antibodies to gliadin which is a "piece" of gluten" in
wheat only. Gliadin corresponds to hordein in barley, secalin in ry,
and avenin in oats. These pieces define the difference between these
grains.
"Celiac only" specialists no longer use this test for celiac diagnosis
because their patients often have these antibodies but no villi damage.
Gluten syndrome
researchers say antigliadin antibodies are very important indicators that the body
is fighting gliadin (wheat) and that the damage caused by the antigliadin
antibodies or other gluten related antibodies may be somewhere else in the body
beside the intestinal villi.
AGA can be checked in 4 places
in the immune system, IgA, IgG, IgM and IgE, hence the following
abbreviations:
AGA-IgA
AGA-IgG
AGA-IgM
AGA - IgE
- This antibody indicates a true "allergic" reaction, (Like a bee
sting or peanut reaction) Therefore this test is usually run only if the
patient's reaction justifies the test. It is used by allergists as a
skin test.
Most standard celiac tests only
test for either AGA-
IgA and IgG, and usually neither.
Researchers who look for a
wider scope of "the gluten syndrome" consider AGA to be important antibodies.
They may
check IgA, IgG and IgM, in order not to miss them.
However,
some patients
do not have any AGA antibodies, but they may have other gluten related
antibodies.
 Close:
a.
AGA - Antigliadin Antibodies
Close:
a.
AGA - Antigliadin Antibodies
 b. Gluten Antibodies -
Why is gluten itself not tested???
b. Gluten Antibodies -
Why is gluten itself not tested???
Gluten - IgA
Gluten - IgG
Gluten - IgM
Note:
These are NOT antigliadin (AGA) tests. Gliadin is a "piece" of gluten.
This tests checks for antibodies to the actual whole
molecule of gluten protein.
Almost no one tests for
gluten!!!! WHY!!
Immunosciences Laboratories, Optimal Resource Labs and ALCAT and ELISA/ACT
Biotechnologies labs test gluten.
 Close
- Gluten Antibodies
Close
- Gluten Antibodies
 c. Gluteomorphins - Immunosciences Laboratories
c. Gluteomorphins - Immunosciences Laboratories
Gluteomorphins are specific pieces of the large gluten molecule
that may form during improper digestion and that are not broken
down enough. Sometimes when gluten is removed from the diet, if the patient
has gluteomorphins that have cross reacted to brain tissue, they may
experience temporary withdrawal symptoms. In some cases this
withdrawal may be quite severe and the patient may experience depression or
psychiatric symptoms.
There is no abbreviation, hence
they are called:
-
Gluteomorphins - IgA
Gluteomorphins - IgG
Gluteomorphins - IgM
The gluteomorphin test is a
blood test available from Immunosciences Laboratories, Los Angeles, CA.
In
published research, gluteomorphin antibodies are reported to cross react/bind/or stick to cerebellar (brain) tissue
and nerves. Their structure is described on
page 191 of this article from the International Journal of
Immunology.
*(In
milk, corresponding peptides are "Casomorphins")
Labs that process gluteomorphin
tests find that some patients have gluteomorphin antibodies instead of
antigliadin antibodies (AGA) and others have both or other antibodies.
Here is a quote from
Dr. Aristo
Vojdani of Immunosciences Laboratories which discusses gluteomorphin antibodies.
"Gluteomorphins are very
small peptides of gluten the size of 8-80 amino acids. When gluten is
broken down by body enzymes to small peptides, some of these peptides bind
to receptors on the brain and immune system cells.
Since usually morphins bind
to these receptors, and gluten peptides also bind to these receptors, these
molecules are then called gluteomorphins, meaning molecules from gluten bind
to morphin receptors and act like morphins. That is why patients with
gluten sensitivity also have neurological involvements."
Aristo Vojdani, Ph.D, M. T.
8/23/2006
References:
Infections,
Toxic Chemicals, and Dietary Peptides Binding to Lymphocyte Receptors and
Tissue Enzymes are Major Instigators of Autoimmunity in Autism
Immune Response to
Dietary Proteins, Gliadin and Cerebellar Peptides in children with Autism
Heat Shock
Protein and Gliadin Peptide Promote Development of Peptidase Antibodies
in Children with Autism and Patients with Autoimmune Disease.
 Close: Gluteomorphins
Close: Gluteomorphins

d.
tTG - Tissue transglutaminase
d. tTG - Tissue
transglutaminase
tTg - IgA, usually now used as
a standard "celiac only" screener test., is an enzyme that binds with gliadin when there is
damage to the intestinal wall or
in som ecases some other tissue
such as brain tissue. Since it is usually a specific
indicator of tissue damage, it has been adopted
by many "celiac only" specialists as a screener test for possible villi
biopsy.
However,
some
studies show that negative tTG
alone does
not accurately rule out celiac disease or the gluten syndrome since tTG is not
involved in all types of gluten reactivitity..
Standard "celiac only" tests
only check
tTG-IgA.
However, in order not to miss
tTG when it is present, some gluten syndrome researchers check for:
tTG-IgA
tTG-IgG
tTG-IgM
Most tTG antibody tests are
blood tests.
Enterolab tests tTG-IgA in stool (as an earlier
and claimed to be more sensitive source.
Research on stool tests has been
announced but is unpublished and unvalidated.) However
public confidence in this test has risen over the 8 years it has been
available. In most cases the results match patient experience.
 c. Close:
tTG - Tissue transglutaminase
c. Close:
tTG - Tissue transglutaminase
 e.
EMA-Antiendomysial Antibodies
e.
EMA-Antiendomysial Antibodies
e. EMA-Antiendomysial
Antibodies
These antibodies are very
specific to celiac villi damage. They are an older version of the tTG
test. The tTG test has largely replaced it.
This test is fairly expensive
and difficult to process and read. EMA is related to tTG and the tTG
test has replaced EMA in most "celiac only" tests.
 Close:
EMA-Antiendomysial Antibodies
Close:
EMA-Antiendomysial Antibodies
f. AGA-tTG antibodies
-
Antigliadin bound to transglutaminase
g. Cross
Reactive Food proteins - Milk (butyrophilins, casein, casomorphins), corn, egg,
soy, yeast, and in some cases coffee, sesame and chocolate may cross react
with gluten due to similar molecular structure.
 Close: ANTIBODY TESTS
Close: ANTIBODY TESTS
 Tissue Damage ANTIBODY Tests and
biopsies
Tissue Damage ANTIBODY Tests and
biopsies
 Pancreas - Glutamic Acid Decarboxylase IgA, IgG, IgM
Pancreas - Glutamic Acid Decarboxylase IgA, IgG, IgM
Pancreas -
Glutamic Acid Decarboxylase
IgA, IgG, IgM
Found in 65% of celiac (villi
damaged)
patients. Indicates damage to the pancreas. How many gluten
syndrome patients with damage elsewhere, NOT the villi have elevated levels
of Glutamic Acid Decarboxylase?

Close:
Glutamic Acid Decarboxylase
 Brain and Nervous system - Myelin Basic Protein (MBP), Cerebellar and
NeurofilNeurofilament
Antibodies, all IgA, IgG, IgM
Brain and Nervous system - Myelin Basic Protein (MBP), Cerebellar and
NeurofilNeurofilament
Antibodies, all IgA, IgG, IgM
Brain and nervous system
- Myelin Basic Protein, Cerebellar and Neurofilament Antibodies, IgA,
IgG, IgM
Nerve sheath or
"insulation" - Myelin Basic Protein, and to cerebellar
Brain cerebellar tissue
- Back base of the brain, controls balance, gait, etc.
Neurofilaments - These nerve cells are often tangled in Alzheimer's
Disease.
These tissues
are particularly susceptible to cross reaction with antigliadin, anticasein
(milk), gluteomorphins, casomorphins, and other food related antibodies.

Close:
Myelin Basic Protein
& Neurofilament Antibodies
Heat Shock Protein -
Involved in temperature related responses
Skin biopsy - biopsy area next to
Dermatitis Herpetiformis lesions
Stomach -
Parietal Cells - B-12 and Hydrochloric acid function
Thyroid -
Thyroglobulin and Thyroid Peroxidase
Villi - biopsy of
duodenal villi. Dx used by celiac focused specialists
Many many more tissue
tests on the way
 Close: Tissue Damage Tests
Close: Tissue Damage Tests
 GENE TESTS
GENE TESTS
GENE TESTS
Gluten related gene tests are either blood or cheek swab tests. The
tests are run either in 1 or 2 part processes. The 2 part process is
more detailed, more sensitive, and more expensive.
There are
3 different opinions
regarding gluten reactive genes.
 Celiac only researchers recognize HLA DQ 2 or 8.
Other non DQ genes are under investigation. Celiac only researchers recognize HLA DQ 2 or 8.
Other non DQ genes are under investigation.
Standard celiac gene tests test for HLA DQ 2 or 8 and report
only positive/negative meaning "yes" or "no" for the presence of these genes,
NOT the actual genes possessed by the patient. HLA DQ 2 and 8 genes
only are
recognized to be associated with "villi damaged" celiac disease at
this time. Other genes not in the HLA DQ locus are under
investigation.
Kimball Labs offers a
2 part process, reports "yes" or no" for the gene tested, and will
additionally report the specific allele numbers of positive tests to the attending
physician upon request.
 Close: Celiac only researchers recognize HLA DQ 2 or 8.
Close: Celiac only researchers recognize HLA DQ 2 or 8.
 Dr. Ken Fine, MD*, recognizes HLA DQ 1, 2, 3, and 8
for the gluten syndrome. *Gastroenterologist,
Dallas, TX Dr. Ken Fine, MD*, recognizes HLA DQ 1, 2, 3, and 8
for the gluten syndrome. *Gastroenterologist,
Dallas, TX
This means, according to
Dr. Fine, that most Caucasians carry at least one predisposing gene for
gluten reactivity. Enterolab offers a one part gene test that reports the patient's specific HLA DQ
alleles. The advantage is that the patient knows his genes and does
not need to be retested if in the future they are linked to the gluten
syndrome. The one part test is less expensive and in some cases less
sensitive than the 2 part test.
Additional genetic information according to Dr. Fine:
Note this is a summary of information on Dr. Fine's website. Below the
summary are the actual quotes.
HLA DQ 1 and 3 and subsets of those genes also predispose to gluten
reactivity, and are found commonly in patients with Microscopic colitis and
rheumatoid arthritis, but not to villi damaged celiac disease.
Possessing 2 copies of gluten reactive genes predisposes the patient to a
higher risk of developing gluten reactivity and that the resultant gluten
reactivity and disease will be worse.
Each parent possesses 2 HLA genes and passes one HLA DQ gene to the
child. Therefore if the parent possesses 2 gluten sensitive genes, one
gluten sensitive gene will pass to the child.
31% of the American population carries the HLA DQ 2 gene
12% of the American population carries the HLA DQ 8 gene
38% of the American population carries the HLA DQ 1 gene
HLA DQ 4 is the only DQ gene which does not appear to predispose to gluten
reactivity according to Dr. Fine. Therefore a person with 2 copies of
HLA DQ 4 (HLA DQ 4,4), a rare combination, is the only combination
that does not predispose to gluten reactivity.
Quotes below reprinted with permission from:
https://www.enterolab.com/StaticPages/Faq_Result_Interpretation.htm
https://www.enterolab.com/StaticPages/Frame_TestToOrder.htm#Genetic_testing
Why are gene results so
complicated, and which genes predispose to gluten sensitivity/celiac sprue?
Gene tests for gluten
sensitivity, and other immune reactions are HLA (human leukocyte antigen),
specifically HLA-DQ, and even more specifically, HLA-DQB1. The nomenclature
for reporting HLA gene results has evolved over the last two decades as
technology has advanced. Even though the latest technology (and the one we
employ at EnteroLab for gene testing) involves sophisticated molecular
analysis of the DNA itself, the commonly used terminology for these genes in
the celiac literature (lay and medical) reflects past, less specific, blood
cell-based (serologic) antigenic methodology. Thus, we report this older
"serologic" type (represented by the numbers 1-4, e.g., DQ1, DQ2, DQ3, or
DQ4), in addition to the integeric subtypes of these oldest integeric types
(DQ5 or DQ6 as subtypes of DQ1; and DQ7, DQ8, and DQ9 as subtypes of DQ3).
The molecular nomenclature employs 4 or more integers accounting together
for a molecular allele indicated by the formula 0yxx, where y is 2 for DQ2,
3 for any subtype of DQ3, 4 for DQ4, 5 for DQ5, or 6 for DQ6. The x's (which
commonly are indicated by 2 more numbers but can be subtyped further with
more sophisticated DNA employed methods) are other numbers indicating the
more specific sub-subtypes of DQ2, DQ3 (beyond 7, 8, and 9), DQ4, DQ5, and
DQ6. It should be noted that although the older serologic nomenclature is
less specific in the sense of defining fewer different types, in some ways
it is the best expression of these genes because it is the protein structure
on the cells (as determined by the serologic typing) that determines the
gene's biologic action such that genes with the same serologic type function
biologically almost identically. Thus, HLA-DQ3 subtype 8 (one of the main
celiac genes) acts almost identically in the body as HLA-DQ3 subtype 7, 9,
or other DQ3 sub-subtypes. Having said all this, it should be reiterated
that gluten sensitivity underlies the development of celiac sprue. In this
regard, it seems that in having DQ2 or DQ3 subtype 8 (or simply DQ8) are the
two main HLA-DQ genes that account for the villous atrophy accompanying
gluten sensitivity (in America, 90% of celiacs have DQ2 [a more Northern
European Caucasian gene], and 9% have DQ8 [a more southern
European/Mediterranean Caucasian gene], with only 1% or less usually having
DQ1 or DQ3). However, it seems for gluten sensitivity to result in celiac
sprue (i.e., result in villous atrophy of small intestine), it requires at
least 2 other genes also. Thus, not everyone with DQ2 or DQ8 get the villous
atrophy of celiac disease. However, my hypothesis is that everyone with
these genes will present gluten to the immune system for reaction, i.e.,
will be gluten sensitive. My and other published research has shown that DQ1
and DQ3 also predispose to gluten sensitivity, and certain gluten-related
diseases (microscopic colitis for DQ1,3 in my research and gluten ataxia for
DQ1 by another researcher). And according to my more recent research, when
DQ1,1 or DQ3,3 are present together, the reactions are even stronger than
having one of these genes alone (like DQ2,2, DQ2,8, or DQ8,8 can portend a
more severe form of
celiac disease).
Is it possible to tell
which parent gave me the celiac or gluten sensitivity
gene?
Everyone has two
copies (or alleles as they are called scientifically) of every gene in the
body; one from mother and one from father. The only way to know if a parent
definitely has a gluten sensitive or celiac gene without testing them
directly, is if a child has two such genes (having received one from mother
and one from father). If only one gluten sensitive or celiac allele is
present in a child, there is no way to know if it came from mom or dad. One
gene is enough, however, to get clinically significant gluten sensitivity or
celiac disease, and from published research, two copies yields an even
stronger reaction and hence, potentially more severe gluten-related
complications.
If I do not have a gluten sensitive or celiac gene, does that mean my
parents/siblings/children do not?
Because everyone has two copies (alleles) of every gene, but a parent only
gives one of these genes to each of their offspring (distributed randomly
between a parent's two alleles), even if a child does not have a gluten
sensitive or celiac gene, one or both parents could have one of these
predisposing genes as their other allele. Hence, a person without a
predisposing gene could still have parents or siblings with these genes. To
be sure, each family individual must be tested to know. (The only certainty
with respect to genetic testing is that if a person is found to have two
predisposing genes, then every one of his/her children and both parents will
have at least one copy of these genes, which is enough to get clinically
significant gluten sensitivity or even celiac disease.) Because a child gets
one allele from each of their parents, even though a particular person does
not have a gluten sensitive gene, their children have a good chance of
getting one from the other parent since these genes are very common (see
next paragraph).
How common are the gluten sensitivity and celiac genes?
DQ2 is
present in 31% of the general American population. DQ8 (without DQ2) is
present in another 12%. Thus, the main celiac genes are present in 43% of
Americans. Include DQ1 (without DQ2 or DQ8), which is present in another
38%, yields the fact that at least 81% of America is genetically predisposed
to gluten sensitivity. (Of those with at least one DQ1 allele, 46% have
DQ1,7, 42% have DQ1,1, 11% have DQ1,4, and 1% have DQ1,9.) Of the remaining
19%, most have DQ7,7 (an allele almost identical in structure to DQ2,2, the
most celiac-predisposing of genetic combinations) which in our laboratory
experience is associated with strikingly high antigliadin antibody titers in
many such people. Thus, it is really only those with DQ4,4 that have never
been shown to have a genetic predisposition to gluten sensitivity, and this
gene combination is very rare in America (but not necessarily as rare in
Sub-Saharan Africa or Asia where the majority of the inhabitants are not
only racially different from Caucasians, but they rarely eat
gluten-containing grains, and hence, gluten-induced disease is rare). Thus,
based on these data, almost all Americans, especially those descending from
Europe (including Mexico and other Latin states because of the Spanish
influence), the Middle East, the Near East (including India), and Russia,
are genetically predisposed to gluten sensitivity. (That is why we are here
doing what we do!) But be aware that if a person of any race has a gluten
sensitive gene, and eats gluten, they can become gluten sensitive.
What type of genetic testing does Enterolab
offer?
https://www.enterolab.com/StaticPages/Frame_TestToOrder.htm#Genetic_testing
In the genetic assessment for
the predisposition to celiac disease (a disease defined as villous atrophy
and inflammation of the small intestine resulting from gluten sensitivity -
the immune response to dietary gluten), the heterodimer HLA-DQA1*0501 and
HLA-DQB1*0201 is one of the main genes required to develop the tissue lesion
of celiac disease. However, it appears from research studies that HLA-DQ1,
HLA-DQ2, and HLA-DQ3 can all lead to immune reactions to gluten (i.e.,
gluten sensitivity) even in the absence of intestinal villous atrophy.
Non-celiac gluten sensitivity syndromes are no less severe than ones
accompanied by villous atrophy, in terms of symptoms they may cause,
accompanying autoimmune diseases in other parts of the body, and resultant
disability. Thus, it is more important to assess for genetic predisposition
to the underlying immune reactivity to gluten itself than just the one
clinical form called celiac disease. Furthermore, fecal analysis cannot
diagnose celiac disease, therefore EnteroLab makes no such claims of doing
so.
In weighing the potential clinical benefit to our clients of adding HLA-DQA1
locus typing (to our current practice of typing only the HLA-DQB1 locus)
versus the almost doubling of cost and price, we have found through internal
research that the frequency wherein HLA-DQ2 positivity is the celiac-related
DQB1*0201 allele verses the non celiac 0202, 0203, 0204, or 0205 alleles is
overwhelming in favor of the celiac 0201 (and we now even separate these
subtypes). By linkage dysequilibrium, HLA-DQA1*0501 will usually accompany
HLA-DQB1*0201. Furthermore, the presence of HLA-DQ2 assessed serologically
(functional presence of any DQ2 gene product) has always shown itself to be
able to bind gliadin, and therefore predispose to gluten sensitivity (even
if someone did not develop celiac disease/villous atrophy). For these three
reasons (the overwhelming prevalence of the 0201 allele of DQ2 in our
clientele, the linkage dysequilibrium of DQA1*0501 with DQB1*0201, and the
greater importance of diagnosing the underlying immune reactivity to gluten,
regardless of syndrome caused), we have decided to keep the price down for
our clients and limit gene testing to the HLA-DQB1 locus. Finally, the
treatment for gluten sensitivity and celiac disease is the same -
complete-strict removal of gluten from the diet. The presence of any gene
predisposing to immune reactivity to gluten (especially when accompanied by
symptoms or an associated clinical syndrome) provides necessary information
to the client to make an informed decision about whether or not to adopt a
gluten-free diet.
 Close: Dr. Ken Fine, MD*, recognizes HLA DQ 1, 2, 3, and 8
Close: Dr. Ken Fine, MD*, recognizes HLA DQ 1, 2, 3, and 8
 Dr. Aristo Vojdani, PhD* believes a gene is
unnecessary but if present will predispose for a gluten response.
*Immunologist,
Los Angeles, CA. Dr. Aristo Vojdani, PhD* believes a gene is
unnecessary but if present will predispose for a gluten response.
*Immunologist,
Los Angeles, CA.
See
Medical Diagrams
Dr. Vojdani of Immunosciences Laboratories reports that non celiac (villi
damage) gluten
intolerance is a serious gluten related reaction that does NOT REQUIRE A
PREDISPOSING GENE. This reaction is triggered by exposure particularly
to toxins, and also stress and infections. (See Medical
Diagrams/Gluten intolerance diagram. Therefore he does not believe
that the gene test is worth the expense.
However: It is the opinion of this website that an inexpensive
gene test is a valuable test in that it often provides supportive
information not only to the patient but to family members. People take
genetic information seriously. Example: A seriously symptomatic patient
tested negatively to incomplete antibody tests and was temporarily
misdirected back to a
gluten containing diet with poor results. Later he did an inexpensive gene test and went gluten
free based on positive genes. He understood they only indicated a predisposition,
but given his obvious reactions to gluten and the gene test he finally "took
the step" to go strictly gluten free. In this case the person's entire life
changed for the better, physically and particularly mentally and
emotionally. Other family members also investigated the issue seriously
as a result of his gene test.
Here is Dr. Vojdani'she editorial paper which mentions his opinions on
genetics.
The Immunology of
Immediate and Delayed Hypersensitivity to Gluten - European
Journal of Inflammation Vol 6 No. 1 1-10 (2008) Editorial - A. Vojdani
Beverly Hills, CA
(now Los Angeles, CA) T. O'Bryan, Warrenville, IL,( now Chicago, Il), G.
H. Kellermann Neuroscience, WI, USA
Full text here
Note: This file contains 2 articles from the
journal.
Scroll to the top to find the Vojdani article.
 Close: Dr. Aristo Vojdani, PhD* believes a gene is
unnecessary.
Close: Dr. Aristo Vojdani, PhD* believes a gene is
unnecessary.
 Close:
Close:
GENE TESTS
 CROSS REACTIVE FOODS TESTS CROSS REACTIVE FOODS TESTSFoods that are
known to have a similar molecular structure to gluten and thought by some
researchers to cross react in some cases with gluten include:
Milk (casein, casomorphins,
butyrophilins) -- IgA, IgG, IgM
Corn - IgA, IgG, IgM
Egg - IgA, IgG, IgM
Soy - IgA, IgG, IgM
Yeast - IgA, IgG, IgM
To some degree also:
Coffee
Sesame
Chocolate
Some gluten
free substitute foods including
Millet
Quinoa
Buckwheat
may also
cause problems for some people who develop multiple food sensitivities.
Here is a quote from Dr Ken
Fine MD, EnteroLab, which discusses these sensitivities.
https://www.enterolab.com/StaticPages/Frame_TestToOrder.htm#What_about_yeast
What about yeast sensitivity?
Although we know less about yeast sensitivity than gluten sensitivty
(because the former has been identified and studied for a shorter period of
time), we now know that it too can be associated with an immune reaction
that damages the intestine and perhaps other tissues in the body. Yeast
sensitivity is the only reaction identified to be present in people with a
devastating intestinal inflammatory disease called Crohn's disease. Through
research, we at EnteroLab have identified coexisting yeast sensitivity in at
least three-quarters of those we find to be gluten sensitive. This is not
surprising since many gluten containing foods also contain yeast (such as
brewer's and baker's yeast). We also find that some people get more symptom
relief from a gluten-free diet when it is also yeast-free.
What about milk, egg, and/or
soy sensitivity?
Since the 1960's, research has shown that people who are immunologically
sensitive to gluten have a higher than average chance of being sensitive to
other dietary proteins, especially to those in milk, eggs, and soy. This can
be detected by antibodies to these dietary proteins, and our patented stool
antibody tests can reveal these to be present before they can be detected in
blood. Sensitivity of the immune system to milk, egg, and soy proteins can
cause intestinal syndromes and damage mimicking that caused by gluten and
celiac sprue. Furthermore, recent research has linked antibodies to milk
proteins to the devlopment of eczema, diabetes, multiple sclerosis, autism,
and other immunologic syndromes.
To encourage people to get the maximum benefit from their testing and their
dietary treatment, for a limited time, EnteroLab is offering the Milk
Sensitivity Stool Test Free when you order the Gluten Sensitivity Stool and
Gene Panel Complete.
Some labs that offer cross
reactive food sensitivities.
www.EnteroLab.com
IgA stool testing of multiple foods beyond milk, egg, yeast, soy - coming
2009
www.ImmunosciencesLabs.com - multiple panels of foods IgA, IgG,
IgM - Not available at this time
www.OptimumHealthResource.com - multiple food IgG antibody panels
www.ALCAT.com - multiple food panels,
cytotoxic test for white cell reaction - A controversial test *
www.ELISAACT.com
ELISA/ACT Biotechnologies-food panels-cytotoxic lymphocyte reaction *
-
Note: Cytotoxic testing is
controversial - Many professionals believe cytotoxic testing simply
identifies foods eaten frequently. Some patients insist these tests
helped them pinpoint problem foods.
 Close: CROSS REACTIVE FOODS TESTS
Close: CROSS REACTIVE FOODS TESTS
 Close: 2. List of tests Close: 2. List of tests
 3. What are
the differences between gluten syndrome and celiac tests? 3. What are
the differences between gluten syndrome and celiac tests?
"Celiac only" tests and
interpretations are less detailed and target only one type of damage.
They look only and very specifically for markers
associated with villi damage in the duodenum for a celiac disease
diagnosis, and gluten free diet.
They test :
-
tTG-IgA as a screener for
biopsy
-
optional: AGA-tTG,
possibly also AGA-IgG
-
IgA deficiency if
necessary (Some people do not make IgA)
-
If in doubt, sometimes the HLA DQ2
and 8 genes
If the blood screeners are
positive, celiac specialists biopsy the villi only for damage. Villi
damage alone (not any other other place in the body) is considered the gold
standard diagnostic tool for celiac disease and the gluten free diet.
(Celiac specialists believe that if a patient insists that gluten bothers
him but they cannot find the few antibodies they test for, or villi damage,
that this reaction is not an immune reaction and is not dangerous.
Other specialists strongly disagree with this opinion because they test
for more antibodies and find them and for damage in other places and
find it.)
Other gluten syndrome specialists now
question this viewpoint but villi focused diagnostic criteria remains
unchanged. Most practitioners are only aware of celiac disease guidelines
only. Furthermore, they only think of this possibility if there are classic gut symptoms.
They do not think of celiac disease as a subset of the gluten
syndrome.
Gluten Syndrome tests are more detailed. They look for:
More antibodies in more places in the immune system. (Gluten,
gliadin. gluteomorphins, tTG, wheat kernel, Total IgA, - all IgA, IgG,
IgM)
Tissue damage in many
places, not just the villi. -
Foods that crossreact with gluten and body tissues.
-
More genes although some think the gene is not necessary.
-
More mediums - blood, stool, saliva
-
See current Immunosciences Labs list on the
Lab Charts page.
Tests not available at this time.
Watch for further announcements on home page of this website.
Gluten Syndrome oriented specialists recommend a gluten free diet
when they find gluten related antibodies above normal limits. They consider
improvement on the gluten free diet conclusive regardless of the particular underlying gluten related process
or area of tissue damage.
Some practitioners use kinesiosiology (muscle testing) or other energy
testing for additional clues. Methods and criteria varies widely between practitioners.

Close:
3. What differences are there between gluten
reactivity and celiac tests?
 4. What test viewpoints exist among today's specialists? 4. What test viewpoints exist among today's specialists?
4.
What test viewpoints exist among today's specialists?
See
Seven Viewpoints Comparison Chart
Celiac specialists
-
Celiac specialist focus on
villi damage only for diagnosis. They believe a person with gluten
damage will always have villi damage. They test blood samples for:
-
tTG enzymes
-
optional: antigliadin
antibody
-
IgA deficiency if
necessary
-
If in doubt, the HLA DQ2
and 8 genes, reported positive/negative
If the screener test is
positive they biopsy for villi damage and only if the biopsy is positive do
they recommend a gluten free diet. Many now question this
viewpoint but celiac villi focused diagnostic criteria remains unchanged.
Villi damaged celiac prevalence is estimated 1:100 in the healthy
population.
Dr. Vojdani, Immunosciences Laboratories
Dr. Vojdani
believes there are many more antibodies to test, and that damage may occur in many places in the body but not necessarily
always to
the villi. Therefore he recommends a complete as possible panel of
gluten related and cross reactive food antibody tests. He also
recommends a panel testing a number of tissues most susceptible to
damage in replace to only one tissue damage test, the invasive villi
biopsy.
He tests many antibodies and
believes they are proof of immune reaction:
-
15 antibodies - Gliadin, gluten
itself, wheat, tTG, and gluteomorphins, all IgA, IgG, IgM (15
antibodies total at this time more coming)
-
Crossreactive foods - milk,
egg, corn, soy, yeast - all IgA, IgG, IgM
-
Neurological and organ damage (cerebellar,
neurofilaments, mylein basic protein, plus thyroid, pancreas, stomach, and
other tissues and functions. He believes gluten and other food
antibodies cross react with and damage many organs and tissues in the
body.(He tests IgA, IgG, IgM)
Dr. Vojdani has a 30% gluten
related positivity rate in his lab. Dr. Thomas O'Bryan tested all his
patients over 4 years with a very complete panel of gluten related
antibodies (over 350 sick patients, with a 77% positivity rate.)
Dr. Ken Fine Enterolab
Dr. Fine believes checking
stool catches the gluten syndrome earlier than blood. He adjusts his tests
for a low level of antibodies usually found in stool.
Dr. Fine checks
stool
for:
AGA-IgA
Ttg-IGA
Intestinal function (this is
his own test)
milk (sometimes free in a combo
package)
Optional - corn, egg,
soy, yeast (IgA)
Optional - gene test, he
reports the patent's actual HLA DQ subtype, 1 step test
A stool test indicates
that there are antibodies in stool, not necessarily in blood, although they may be also
present in blood or could be present in blood in
the future. Dr. Fine considers high stool antibody levels
indicative of gluten reactivity. See Enterolab on
Lab Charts page or www.enterolab.com
Dr. Fine's test has a high
positivity rate as follows compared to 1% celiac test positivity rates.
62-69% positive-common
symptoms (autoimmune, fatigue, headache, digestive, etc.)
44% positive
for non digestive, non specific symptoms
28% for
non symptomatic (silent symptom) patients
 Close:
4. What test viewpoints exist among specialists?
Close:
4. What test viewpoints exist among specialists?

Close: B. Understanding gluten
reactivity tests
and also tests specific to the villi damaged "celiac" subset of the
gluten syndrome.
 C.
How to choose? Should I pay for more than one test
if my first test is negative and I question it?
C.
How to choose? Should I pay for more than one test
if my first test is negative and I question it?
 1. Which test or tests are best in my case?
1. Which test or tests are best in my case?
The purpose of the test and the patient's circumstances matter.
Example: A patient who
has discontinued eating gluten may no longer have
detectable antibodies in the blood stream, ruling out a blood antibody test
for diagnosis. But if the same patient is already diagnosed and wants to
check his diet compliance, a low antibody count
indicates a "clean" gluten free diet.
What information are you looking for?
 If you currently eat gluten and need a
diagnosis:
If you currently eat gluten and need a
diagnosis:
Gluten Syndrome specialists advise:
Test as many gluten related antibodies as necessary or as possible (15
approximately). If a positive is obtained, remove gluten. If
negative, the tests are inconclusive since there are more antibodies than
there are tests. (This is uncommon if all known antibodies are run.)
Gluten - IgA, IgG, IgM
Gliadin - IgA, IgG, IgM
Gluteomorphins - IgA, IgG, IgM
Wheat - IgA, IgG, IgM
tTG - IgA, IgG, IgM
Also test and remove other cross reactive foods.
Milk (Butyrophilins, Casein, Casomorphins- IgA, IgG, IgM)
Corn - IgA, IgG, IgM
Egg - IgA, IgG, IgM
Soy - IgA, IgG, IgM
Yeasts, Molds, Fungus - IgA, IgG, IgM
Test and treat damage in susceptible tissues
with
tissue damage tests or "predictive
antibodies" for many tissues (not just villi) These tests
replace a villi biopsy unless there are other reasons to biopsy.
Brain, nervous system - Cerebellar, neurofilaments, myelin basic protein
Pancreas - Glutamic Acid Decarboxylase
Heat Shock Protein
-
Involved in temperature related
responses
Skin biopsy
- biopsy area next to
Dermatitis Herpetiformis lesions
Stomach
-
Parietal Cells - B-12 and Hydrochloric acid function
Thyroid -
Thyroglobulin and Thyroid Peroxidase
Villi
- biopsy of
duodenal villi. Dx used by celiac focused specialists
Skin - This is a relatively
easy biopsy if DH appears to be present.
Many many more tissue tests on
the way
Test for nutrient deficiencies, calcium, iron, B 12, vitamin D, etc.
Celiac specialists advise: See
Lab Charts page for website links
tTG -IgA screener, if positive biopsy the villi. May run tTG - IgG,
or possibly Gliadin IgA, IgG
Villi biopsy
- If the biopsy is positive
start the gluten free diet. If negative, remain on a gluten diet.
Some practitioners also check tTG-IgG, gliadin IgA, IgG and
occasionally EMA antibodies. Some practitioners vary in their dietary
recommendations depending on the situation.
Gene test
(optional) To check for predisposition if there is uncertainty.

Close : If you are currently on a gluten containing diet
 If you are not on a gluten containing diet
If you are not on a gluten containing diet
You have 4 choices
Enterolab tests work for several months after the gluten free diet is
established. Call the lab for further advice. Enterolab tests 2
gluten antibodies in stool, claimed to be a more sensitive medium than blood
ELISA/ACT Biotechnologies requires 1 serving of gluten in the past 6 months.
This test checks wheat, gluten, gliadin and several other gluten grains for
lymphocyte reaction.
ALCAT does not require a gluten containing diet at all. This test checks
white cells for general adverse reaction. This test is controversial.
Some professionals believe this test only shows the foods eaten frequently.
Some patients believe this test helped them pinpoint their problems foods
and substances.
Gene test (optional) to check for predisposition.
 Close: If you are not on a gluten containing diet
Close: If you are not on a gluten containing diet
 If you want to check your diet compliance If you want to check your diet compliance
Gluten Syndrome specialists:
Test all gluten related and cross reactive antibodies IgA, IgG, IgM.
(Sometimes cross reactive antibodies, particularly yeast, may keep gluten
antibodies high even on a clean GF diet.)
Celiac specialists: See
Lab Charts page for website links
Usually test gliadin and tTG antibodies.
In some cases they may rebiopsy to evaluate villi healing.
 Close: If you want to check your diet
compliance
Close: If you want to check your diet
compliance
 If you are on a strict gluten free diet with little or no improvement. If you are on a strict gluten free diet with little or no improvement.
Gluten syndrome specialists:
Check the diet for hidden gluten
Test for cross reactive food reactions including particularly yeast, mold,
and fungal infections, gut flora imbalances, nutrient imbalances including
particularly calcium, iron and B 12, toxins, parasites, other non gluten
related conditions.

Audio-Dr. Thomas
O'Bryan, DC, CCN DACBN, Chicago,
IL
"What
to do if I'm gluten free but I don't feel great."
January, 2009,
Wheaton, IL
www.thedr.com
Celiac specialists:
Test for gluten free diet compliance, nutrient deficiencies and non gluten
related conditions. Here is a
protocol recommendation for celiacs from Dr. Stephen
Holland, MD, Naperville, IL
 Close: If you are on a strict GF diet with little or no improvement.
Close: If you are on a strict GF diet with little or no improvement.
Summary descriptions of test options.
See
Lab Charts.
Common Celiac test panels usually only test tTG and sometimes gliadin
(wheat) and are available from several labs.
See
Lab Charts. They all are blood tests
and require that the patient remain on a gluten diet until the test is
performed.
The Immunosciences Celiac Neuroautoimmune Panel is the
most detailed blood antibody panel available. It requires that a patient
be on a
diet containing the foods tested, including gluten.
It checks the most gluten related antibodies in the most places.
It checks a number of other cross reactive food protein antibodies.
It checks many susceptible body/organ tissues for damage or
predictive
antibodies.
Tests not available at this
time. Watch home page of this website for further information.
The Enterolab Stool Panels claim to work for a while
after the patient has discontinued gluten. It also claims to be more
sensitive than blood tests, that is, to detect
levels of gluten related antibodies earlier than blood tests.
Optimum Health Resources 96-food IgG panel checks gliadin (wheat) AND
gluten and other gluten grains. They all require a gluten
containing diet.
The
ALCAT panels do not
require a gluten containing diet, and are therefore the
only blood test option for patients who have not eaten gluten for years.
These panels test a large number of foods and other substances. It is a
controversial test. Some believe it only shows the foods eaten most
frequently.
The ELISA/ACT Biotechnologies test
requires a serving of gluten within the past 6 months. It tests
lymphocyte (special white cells that make the antibodies) reaction.
The gluten or grain is exposed to the lymphocytes and the lymphocytes swell
and a halo forms around them just prior to when the antibodies burst out of the cell.
Gene tests determine if a patient is
predisposed to a gluten related reaction. They do not indicate the
patient currently reacts to gluten. Gene tests can provide helpful
information to family groups beyond the individual tested.
They are run in 1 or 2 part processes. The 2 part step is more
sensitive for a small number of patients.
Gene tests use either blood or cheek swab.
A gluten diet is not needed for the test.
Prometheus, Kimball and Enterolab run them in a wide price range.
Results are reported 2 different ways depending on the lab.
Either the report is "Yes or No" for HLA DQ 2 or 8, or the patient is told
which HLA genes he actually possesses regardless of whether they are HLA DQ 2 or 8.
(For instance, he may possess HLA 1 and 3, or 3 and 4. Labs that
report only 2 and 8 would simply report "negative 2 or 8" for these
patients.)
Experts differ on the primary genes involved and more genes in other
sections of DNA are under study. Therefore some patients wish to know
which actual HLA genes they possess since more HLA genes are already
fingered by Dr. Fine and may be more generally recognized in the future.
-
"Celiac only" specialists only recognize villi damage and
the HLA DQ 2 and 8 genes, for predisposition to villi damaged celiac disease
(present in 43% of the Caucasian population). Prometheus and Kimball
Labs offer 2 part gene tests and report "yes" or "no", positive/negative for
the HLA DQ 2 and 8 genes only.
He recognizes HLA DQ
2 and 8 for celiac villi focused damage and HLA DQ 1 and
3 for non celiac gluten syndrome reaction. Combined, these 4 genes and
subtypes are present in 83% of the Caucasian population.
He believes HLA DA 4 is the only non gluten reactive
genotype. Therefore he believes only a HLA DQ 4, 4 patient (double copy of DQ 4) is
not predisposed to a gluten reaction. His lab has processed very very few
positive gluten syndrome tests from patients with DQ 4, 4 genotype.
He believes that if gluten related antigens are presented to the immune
system (ie, slip past the gut wall before they are properly digested), a
person with a gluten reactive gene will react.
-
Dr. Vojdani, Immunosciences
Laboratories
believes the gluten
intolerance reaction is autoimmune,
(see Medical Diagrams) and DOES NOT REQUIRE A
GENE. He believes anyone regardless of genetic predisposition can develop the
autoimmune gluten intolerance reaction
from exposure to stress,
, and infections.
Therefore according to Dr. Vojdani, a negative test does NOT rule out
serious gluten intolerance reactions. Dr. Vojdani only considered HLA DQ 2 and 8,
not 1 and 3 and their subtypes when he formulated this hypothesis.
Immunosciences does not run the gene test.
No Immunosciences tests are
available at this time. Watch the home page of this website for
further information.
Many patients find that a positive gene test encourages family members to
seriously consider the possibility of the gluten syndrome.
Energy tests - There are various energy related tests
including various forms of
kinesiology (muscle testing) or
electroaccupuncture
according to Voll that may not require a gluten diet. Consult alternative
practitioners for information.
 Close: 1. Which test or tests are best in my case?
Close: 1. Which test or tests are best in my case?
 2. Are there risks or alternatives particularly if the test is invasive? 2. Are there risks or alternatives particularly if the test is invasive?
2. Are there risks or alternatives particularly if the test is
invasive?
Gluten syndrome blood, stool
and gene tests themselves are minimally invasive (blood draw). The
risk or challenge lies in finding tests that catch the particular
antibodies or markers that the patient carries. An inadequate, inaccurate
negative test may mislead the patient into a false sense of security.
Update
Jan 2009,
A test panel is proposed to include all available gluten related antibodies performed in a
"progressive" manner until a positive result is obtained or all available
options are exhausted. A similar complete test panel has already shown to
pick up at least one positive in 77% of
Dr. Thomas O'Bryan's patients over a 3-4
year period. Watch the home page of this website for further
announcement of this proposed panel. (There are known antibodies for which no tests are
developed so a negative panel is inconclusive. A false negative is
less likely if more antibodies are tested.)
The celiac villi biopsy is invasive
and therefore carries a some risk although it is performed routinely
today. A known risk is that a negative biopsy may mislead the
patient away from a gluten free diet when in fact real damage may be located
somewhere else beside the villi. Gluten syndrome researchers believe the villi biopsy is NOT a gold
standard for the gluten syndrome, although it is helpful in detecting tumors, or
other abnormalities, and diagnosis of the few patients who in fact happen
to have villi (celiac) damage.
Some researchers therefore consider that antibody tests are more
appropriate alternatives than villi biopsy for diagnosis of gluten
reactivity.
IF A PATIENT HAS ALREADY EXPERIENCED IMPROVEMENT ON A GLUTEN FREE DIET
MANY PATIENTS AND DOCTORS BELIEVE THAT IS A RELIABLE DIAGNOSIS.
PATIENTS OR THEIR FAMILIES
TEND TO SECOND GUESS THIS TYPE OF ELIMINATION DIET DIAGNOSIS, WHICH MAY
LEAD TO LACK OF FAMILY SUPPORT AND RISKY INCOMPLIANCE ISSUES.
CHEATING IS NOT OK REGARDLESS
OF METHOD OF FORMAL DIAGNOSIS OR LACK OF DIAGNOSIS. OVER TIME
REPEATED OCCASIONAL GLUTEN EXPOSURE APPEARS TO HAVE LED TO KNOWN SERIOUS
NEUROLOGICAL AND PSYCHIATRIC HARM IN SEVERAL CASES. IT IS WELL KNOWN IN THE GLUTEN SYNDROME COMMUNITY THAT
A GLUTEN MISTAKE IS USUALLY UNCOMFORTABLE AT BEST. HOWEVER IN SOME
CASES SYMPTOMS MAY BE SILENT OR HIDDEN OR SIGNIFICANTLY DELAYED, AND LEAD
CHEATERS TO A FALSE SENSE OF SAFETY.
 Close: 2. Are there risks or alternatives particularly if the test is invasive? Close: 2. Are there risks or alternatives particularly if the test is invasive?
 3. Is the test necessary?
3. Is the test necessary?
Is the test necessary?
If the patient knows he/she has problems with gluten and improves on a
gluten free diet then many patients and doctors believe that is adequate
proof that the diet is needed regardless of
no test
(inadequate) NEGATIVE tests. In this case, the patient must
commit to a strict GF diet without test confirmation, knowing that the
body's message is it's own confirmation.
Antibody Tests
Celiac specialists use tTG antibodies to screen for those patients
who should be scoped for villi damage. Therefore they believe blood
tests are a necessary first step in the celiac diagnosis process.
Gluten Syndrome researchers say that a positive gluten related antibody test confirms
that the immune system reacts to gluten. A positive helps the patient and
family take the condition seriously and strictly comply with the gluten free diet, especially in social situations. This is particularly true for
kids who as teens may question their need for the diet if there is no test,
or maybe even if there was an initial positive test.
HOWEVER THIS IS NOT A REASON TO TRY A GLUTEN CHALLENGE*
Late teens and
20's carry a higher risk for symptoms to surface
including serious neurological symptoms. A challenge at that age or
any age is a grave risk, but symptoms may or may not not show up immediately.
Delayed or silent reactions may mislead a teen or anyone into thinking they
are OK, or "outgrew" the reaction.
* A gluten challenge means the a patient who is already strictly gluten free
decides to resume eating gluten for a period of weeks or months in order to
be tested for an immune reaction to gluten.
Villi Biopsy
Celiac researchers believe a villi biopsy is necessary for diagnosis and gluten
free recommendation.
Gluten syndrome researchers believe a villi biopsy for recommendation of a
gluten free diet is often pointless or misleading since
many patients' damage is elsewhere and not necessarily to the villi.
They believe a negative biopsy is meaningless since damage could be
elsewhere in the body, although a
positive biopsy usually does indicate gluten related damage. However,
a biopsy may be
necessary for other reasons. Gluten syndrome researchers use
"predictive antibodies" and other tests to look for tissue damage in many
places in the body.
 Close:
3. Is the test necessary?
 4. Should I test for other food reactivities and cross reactions
also? 4. Should I test for other food reactivities and cross reactions
also?
Should I test for other food reactivities and their cross reactions at the same time?
Many patients react to several food proteins or to yeast. These proteins tend to
"look alike" and cross
react so some professionals think it makes sense to test for other foods at the same time.
It is suspected that if the patient stops eating one food, but still reacts to another, antibodies to
the food they discontinue (gluten) may continue to produce, and damage
tissue due to the presence of the other reactive foods (egg, milk, soy,
corn, yeast and others).
Published research*
indicates that cross reactions between various protein peptides (pieces) occur through
cellular mimicry. (Simple explanation: This is illustrated by
picturing strings of necklaces
with various patterns of bead colors. The necklaces represent peptides,
which are partly broken down parts of food proteins or other proteins.
The
individual beads represent individual amino acids bound in a string. Sometimes
a
sequence of just
a few "colors" (amino acids in the peptide string) match up enough between the two
different food proteins to cause antibodies to one peptide to "misrecognize" a
similar
peptide and bind/cross react inappropriately to it. In
other words, if a person reacts to one food, they may also react to another
food that "looks like it", meaning it has a slightly similar protein sequence.
So all the cross reactive foods may need to be removed before the immune reaction calms down.
Many practitioners believe
the "leaky gut" or other faulty mucosal barrier needs to be healed to
prevent these peptides from slipping through the gut or other body barriers
before they are broken down enough.
* Reference:
In Celiac Disease, A Subst of Autoantibodies against Transglutaminase Binds
Toll-Like Receptor 4 and Induces Activation of Monocytes
Published Sept 19, 2006 Click for
abstract and full text
Giovanna Zonomi1, Niccardo Navone2, Claudio
Lunardi2, Giuseppe Tidente1, Carerina Bason2,
Simona Sivori3, Buggero Beri2 Marzia Dolcino4,
Enrico Valletta5, Roberto Corrocher2, Antonio Puccetti3,4
1. Section of Immunology, Department of Pathology, Universtiy of Verona,
Verona, Italy,
2. Section of Internal Medicine, Department of Clinical and Experimental
Medicine, University of Verona, Verona, Italy
3. Section of Histology, Departmant of Experimental Medicine, University of
Genova, Genova, Italy
4. Immunology Unit, Institute G. Gaslini, Genova, Italy,
5.Department of Pediatrics, University Hospital of Verona, Verona, Italy
 Close: 4. Should I test for other food reactivities and
cross reactions
Close: 4. Should I test for other food reactivities and
cross reactions
also?
 5. If my test
is negative and I question it, should I try another type of test? 5. If my test
is negative and I question it, should I try another type of test?
5. If my test is negative and I question it, should I try another
test?
A properly run positive test indicates an immune reaction, but no one test
"covers all the bases" so to speak, so a negative is always inconclusive.
To "cover more bases" patients can try more testing of different antibodies,
different mediums, or different types of reactions such as lymphocyte or
white blood cell reactions. See
Testing page to view charts of the following tests and lab
information.
Here is a list of characteristics of the following tests.
Standard "celiac only" blood tests check one or two blood
markers, tTG and sometimes gliadin. They also do not test
for organ damage and other cross reactive food intolerances that can keep gluten antibodies running high even on the gluten free diet.
Cost: varies from $76 for a single tTG screener to about $300 for a
standard panel.
The ALCAT test exposes white blood
cells to various foods and then observes any cell reactions, such as
granulation, swelling, etc. These reactions could be for a number of
reasons, not just presence of antibodies. They simply indicate that the patient's
body does not "like" this substance. ALCAT tests wheat (the whole
kernel), gliadin and gluten, in panels that include many other foods
and substances. This is a home test and does NOT require a gluten
containing diet.
The
Enterolab stool test is a research test that checks
gliadin, tTG and intestinal function in stool*, an earlier location than any blood test,
which likely accounts for its high percentage of positive results. Enterolab also offers other food tests
and a gene test.
This test is a home test and usually works for a while after gluten is
removed from the diet.
*The reference range accounts for an expected number of antibodies that
normally occur in stool.
Immunosciences Celiac Panel checks blood levels of gliadin, tTG AND gluteomorphins,
gluten, and wheat, all for IgA, IgG, IgM.
Tests not available at this
time. Watch home page of this website for further information.
(January, 2009 -
Tests not available at this
time. Watch home page of this website for further information.
Optimum Health Resource Laboratories offers a 96-food IgG
blood panel that includes both gliadin, gluten (gluteomorphin), and 9
other grains. It is a home test and requires a gluten containing diet. Cost:
$379
If the Enterolab test is negative, other listed panels may provide further detail
due to a wider variety of antibodies checked. The patient must
remain on gluten until all tests are complete.
If the Immunosciences blood tests
(not available at this time)
and/or Optimum Health Resource blood tests are negative, the Enterolab
stool test
may catch earlier signs of a gluten reaction. Enterolab tests may be
performed for an unspecified length of time (several months, call the lab to
ask) after the patient is gluten free.
If a patient has been gluten free for a long time, their only choice is the
ALCAT test or a saliva or energy based test offered by alternative
practitioners. Opinions vary regarding the reliability of the ALCAT
test. The ELISA/ACT Biotechnologies requires one serving of the gluten
containing food within 6 months of the test.
 Close: 5. Should I try more than one kind of test?
Close: 5. Should I try more than one kind of test?
 6. I'm considering cutting out gluten without bothering to test. 6. I'm considering cutting out gluten without bothering to test.
6. I'm considering cutting out gluten without
bothering to test.
In this case, consider the following:
It is uncommon, but possible that if you even test extensively you may never
get a positive, and yet you may be very reactive to gluten. The test
you need may not be developed yet.
If you have a family that supports your decision and you are convinced to be
strict without a test, then you are in a favorable situation to skip
testing. However:
-
It's easier for the patient, spouse and family to comply with the gluten free diet if the patient has tested
positive. This is
also particularly true for teens who were put on a gluten free diet as
children and do not remember
how sick they were before the GF diet. Without test results they may
give up the diet just at an age that is
high risk to develop problems. (They may do this even with previous
positive test results.)
In this case, with no test or a negative test that you do not agree with,
simply tell your friends that you are gluten free. Period! Don't mention testing. Testing is
your business, not theirs. If your family, spouse, parents, give you a
hard time, just say "No thanks, I don't do gluten.", and stop talking.
No need to defend your decision. The more you say, the more
opportunity they have to wear you down. They will accept a firm, quiet
but decisive attitude better and quicker in the long run.
 Close: 6. I'm considering cutting out gluten without bothering to test.
Close: 6. I'm considering cutting out gluten without bothering to test.
 Close: C.
How to choose? Should I pay for more than one test to confirm from several directions?
Close: C.
How to choose? Should I pay for more than one test to confirm from several directions?
Testing FAQ's
Note: Due to the high number
of expand/collapse links on this page it is recommended that the reader
close each link as each section is read to keep the page clean and make it easier to
relocate information.
 1. I received my standard antibody/biopsy/gene test results and they are
negative. But I get sick when I try to go back to gluten grains. My
doctor scolded me and my family thinks I'm silly to avoid gluten
because my tests are negative. Help! Why!! I feel deserted.
1. I received my standard antibody/biopsy/gene test results and they are
negative. But I get sick when I try to go back to gluten grains. My
doctor scolded me and my family thinks I'm silly to avoid gluten
because my tests are negative. Help! Why!! I feel deserted.
1. I received my
standard antibody/biopsy/gene test results and they are negative.
But I get sick when I try to go back to wheat/gluten grains. My doctor
scolded me and my family thinks I'm silly to avoid wheat/gluten
because my tests are negative. Help! Why!! I feel
deserted even by the celiac community.
In this case, it is important to
read the information on this website and understand the testing
limitations.
If patients feel better, they decide to believe their body and be firm with doctor, friends and
family. They just say, "no thanks, I don't do gluten!" and stop talking.
They find the more they talk the more friends or family can argue.
They go to a support group on a regular basis and network with
others in their situation for moral support.. They sign up for some of the
online forums for daily info and support. Many many people at the
support groups and the online forums are negative testers and
they know very well they cannot do gluten at all, just like you.
To repeat:
Today's gluten syndrome/celiac testing methods are still very incomplete.
Gluten breaks down into a number of pieces for which there actually are
tests but few labs run them. It also breaks into known pieces for
which there are no tests developed yet. Today's incomplete test panels
appear to produce many more false negatives than true positives.
To repeat once more:
It is helpful to
remember some reasons your test may have been false negative:
You may
have antibodies the test did not check
You may
have damage somewhere else beside the villi.
Some
researchers say toxins can cause the syndrome without the genes. And
some researchers recognize genes that others do not.
Your tests may be been improperly performed.
 Close: 1. I received my standard antibody/biopsy/gene test results and they
are negative.
Close: 1. I received my standard antibody/biopsy/gene test results and they
are negative.
 2. Who is Dr. Ken Fine and what
about his Enterolab
stool and gene tests?
2. Who is Dr. Ken Fine and what
about his Enterolab
stool and gene tests?
2. Who is Dr. Ken Fine and what about his Enterolab stool and gene tests?
In addition to the information
on this page, here is the ClanThompson.com review of Dr. Fine's recent announcement conference
by Lani K. Thompson
titled "News: Celiac Disease, Just the Tip of the Iceberg."
This is a long discussion. As
I researched for testing/treatment for our family beginning in 2003 I
spent some time investigating this topic. I questioned very
experienced people in the celiac support community who know Dr. Fine.
Their stories all matched. Dr. Fine's 8 year long research is not
officially published but his research announcement, a precursor to
publishing, took place March, 2006.
Dr. Fine's website
explaining his work is
www.Enterolab.com.
I divided my reply into three
topics.
 A. Dr. Fine's tests, his
professional career and himself.
A. Dr. Fine's tests, his
professional career and himself.
 Dr. Fine's gene test
Dr. Fine's gene test
Dr. Fine's gene test
I communicated with Kimball
Genetics more than once regarding genes and Dr. Fine's gene test. The
Kimball counselors are wonderful! They state that Dr. Fine's gene test is a credible
test. It is a one part test. Kimball uses a two part test and a different gene classification system so the
counselor was not familiar with the more detailed system Dr. Fine uses.
Dr.
Fine considers DQ 2, DQ 8, and most subsets of DQ 1 and DQ 3 to be
gluten sensitivity genes. He identifies which HLA-DQ gene alleles are
present in the specimen, instead of reporting "positive/negative for DQ 2 or DQ 8.
This gives the patient more exact information regarding his own specific
genes. (Celiac researchers oly recognize HLA DQ 2 and 8 and there are
more they are working on in other areas.)
Dr. Hadjivassiliou from England
is another researcher who has published work on DQ 1.)
Dr. Fine discusses his gene
interpretations at length on his website in his FAQ's and the Research and
Education slides (slide 36)
http://enterolab.com/StaticPages/Faq_Result_Interpretation.htm
http://www.enterolab.com/Lecture/Lecturenew/frame.htm
 Close: Dr. Fine's gene test
Close: Dr. Fine's gene test
 Dr. Fine's fecal antibody and intestinal malabsorption tests
Dr. Fine's fecal antibody and intestinal malabsorption tests
Dr. Fine's fecal antibody and
intestinal malabsorption tests
(This is a fat malabsorption
test Dr. Fine developed to check overall function of the
intestine. He believes that villi damage is not the only type of gut/other
injury that may occur. For instance, instead of villi damage,
neurological signaling mechanisms that control wave like contractions (peristalsis)
that move gut contents may be damaged.
-
Milk, soy, egg and yeast
antibody tests are also available
-
Microscopic colitis stool tests
(lactoferrin) are available.
 Close:
Dr. Fine's fecal antibody and intestinal malabsorption tests
Close:
Dr. Fine's fecal antibody and intestinal malabsorption tests
 Dr. Fine's professional and personal history
Dr. Fine's professional and personal history
Dr. Fine's professional and personal history
Dr. Fine's Curriculum Vitae
Dr. Fine is a qualified
gastroenterologist/professor who helped design the landmark 5 year Fasano
celiac prevalence
study. He formerly taught at Baylor University, and while
still under the auspices of Baylor he took up the unfinished work of retired
English researchers Dr. Michael Marsh and the late Anne Ferguson. (Note: Dr.
Marsh originated the
Marsh classification system of
villi damage, but his
main research project was a gluten sensitivity stool test. No one could
duplicate his work. He lost his grant and lack of validation left his work unfinished
and unusable in many professional's opinions.) Dr. Fine tackled Dr. Marsh's
project from a different direction and from his own observations eventually
grasped the magnitude of gluten syndrome prevalence in the United
States. He left his professorship and research at Baylor, applied for a
patent, and set up an independent accredited lab which offered an affordable
non scripted gluten syndrome stool panel and gene test directly to the public via
internet. Until recently, attempts to
duplicate Dr. Fine's work were also unsuccessful but now research on a
similar note is published. Some research
supports Dr. Fine's work and
one
study does not. Dr. Fine disagrees with methodology used by the
dissenting researchers. Dr. Fine also started a non profit organization,
Intestinal Health
Institute
for educational purposes.
In absence of published
validation I inquired about Dr. Fine's character. He is a "maverick"
in a nice way. He has 3 apparent interests...his gastroenterology, his music,
and helping people. He appreciates spirituality and a simple lifestyle ie.,
he prefers to sing under the stars with a campfire and backpack and societal norms don't necessarily shape his lifestyle.
Dr. Fine suffers chronic health challenges himself and practices a simple
diet that is gluten free. He recommends a
healthy lifestyle.
Everyone in the experienced
support community whom I questioned, "Is this guy really a good guy, or does
he just want me to think so?" says he is sincere,...a good person doing "his
thing" to help others and there are high hopes that he is "on to something"
with his ideas and testing methods.
His recent research announcement and anticipated publishing of his research papers may
contribute greatly to the gluten syndrome community.
(By the way, all our
doctor heroes are "nice guys" who've sacrificed and
taken a beating to bring
the gluten syndrome to our attention.)
In my search I
was reminded by naysayers that Dr. Fine makes money. To be fair I don't know a good
medical pro who does not. They all worked for it. However, in my
investigation I communicated with several who knew him from his position at
Baylor before he began his current research. It is well known locally
that after Dr. Fine chose to operate independently he personally chose an
unusually humble lifestyle, preferring to fund his research and bring
affordable testing directly to the public. I found his lab in a decent
but unostentatious, no frills facility.
Finally, other professionals
beside Dr. Fine report a very high prevalence of NON "villi damaged"
gluten syndrome reactivity. They observe that non celiac gluten syndrome is as serious
or worse than villi damaged celiac disease. Some
of those professionals' conclusions are reported elsewhere on this page.
 Close: Dr. Fine's professional and personal history
Close: Dr. Fine's professional and personal history
 Close: A. Dr. Fine's work,
his professional career and himself.
Close: A. Dr. Fine's work,
his professional career and himself.
 B. Summary of Dr. Fine's announced conclusions
B. Summary of Dr. Fine's announced conclusions
 More gluten syndrome genes
More gluten syndrome genes
Dr. Fine identifies more
gluten syndrome genes than do conservative celiac specialists.
Quote from Dr. Fine's website:
DQ2 is present in 31% of
the general American population. DQ8 (without DQ2) is present in another
12%. Thus, the main celiac genes are present in 43% of Americans. Include
DQ1 (without DQ2 or DQ8), which is present in another 38%, yields the fact
that at least 81% of America is genetically predisposed to gluten
sensitivity. (Of those with at least one DQ1 allele, 46% have DQ1,7, 42%
have DQ1,1, 11% have DQ1,4, and 1% have DQ1,9.) Of the remaining 19%, most
have DQ7,7 (an allele almost identical in structure to DQ2,2, the most
celiac-predisposing of genetic combinations) which in our laboratory
experience is associated with strikingly high antigliadin antibody titers in
many such people. Thus, it is really only those with DQ4,4 that have never
been shown to have a genetic predisposition to gluten sensitivity, and this
gene combination is very rare in America (but not necessarily as rare in
Sub-Saharan Africa or Asia where the majority of the inhabitants are not
only racially different from Caucasians, but they rarely eat
gluten-containing grains, and hence, gluten-induced disease is rare). Thus,
based on these data, almost all Americans, especially those descending from
Europe (including Mexico and other Latin states because of the Spanish
influence), the Middle East, the Near East (including India), and Russia,
are genetically predisposed to gluten sensitivity. (That is why we are here
doing what we do!) But be aware that if a person of any race has a gluten
sensitive gene, and eats gluten, they can become gluten sensitive.
 Close:
More gluten syndrome genes
Close:
More gluten syndrome genes
 Site(s)
of gluten syndrome damage are somewhat gene driven.
Site(s)
of gluten syndrome damage are somewhat gene driven.
Site(s) of gluten syndrome damage
may be
somewhat gene driven.
Quote" My and other
published research has shown that DQ1 and DQ3 also predispose to gluten
sensitivity [reactivity] , and certain gluten-related diseases (microscopic colitis for
DQ1,3 in my research and gluten ataxia for DQ1 by another researcher.
 Close: Site(s) of
gluten reactivity damage may be somewhat gene driven.
Close: Site(s) of
gluten reactivity damage may be somewhat gene driven.
 Villi
may be damaged with DQ 2 or 8 AND a couple of other genes. Villi
may be damaged with DQ 2 or 8 AND a couple of other genes.
Villi damage appears to develop in
cases when HLA DQ 2 or 8 are present in conjunction with a couple of other
genes.
Quote
"it seems for
gluten sensitivity [reactivity] to result in celiac sprue (i.e., result in villous
atrophy of small intestine), it requires at least 2 other genes also.
Thus, not everyone with DQ2 or DQ8 get the villous atrophy of celiac
disease."
 Close:
Villi damage appears to develop... Close:
Villi damage appears to develop...
 Negative stool tests usually accompany negative
genes.
Negative stool tests usually accompany negative
genes.
Dr. Fine stated in his Q and
A at the end of his research announcement that in his
experience negative antibody stool tests processed in his lab are associated with absence of any gluten
syndrome gene. (Exceptions are 1 in 500.)
This statement was made at the Q
and A session at the end of the research announcement in March 2006, and is
available on the DVD of that session. order form ww.enterolab.com
 Close: Dr. Fine stated in his Q and A...
Close: Dr. Fine stated in his Q and A...
 One One
gene is enough. Two, particularly certain pairs, are often worse.
Dr. Fine and others report that one
gene is sufficient to develop gluten reactivity. The presence of
two genes, particularly certain pairs, predispose the patient to more
severe symptoms.
One gene is enough, however, to
get clinically significant gluten sensitivity [reactivity] or celiac disease, and from
published research, two copies yields an even stronger reaction and hence,
potentially more severe gluten-related complications.
Having two copies of a gluten
sensitive [reactive] gene, means that each of your parents, and all of your children
(if you have them) will possess at least one copy of the gene. Two copies
also means there is an even stronger predisposition to gluten sensitivity
[reactivity]than having one gene and the resultant immunologic gluten sensitivity
[reactivity] may be
more severe.
Other research:
http://www.ihop-net.org/UniPub/iHOP/pm/7658236.html?pmid=
Tissue Antigens. 1993 Apr;41(4):173-7
On the HLA-DQ(alpha 1*0501, beta 1*0201)-associated susceptibility in
celiac disease: a possible gene dosage effect of DQB1*0201.
Ploski R,
Ek J,
Thorsby E,
Sollid LM. Institute of
Transplantation Immunology, University of Oslo, National Hospital, Norway
 Close:
Dr. Fine and others report that one gene is sufficient to develop gluten
sensitivity [reactivity]...
Close:
Dr. Fine and others report that one gene is sufficient to develop gluten
sensitivity [reactivity]...
 One
gene equals 50% chance for kids. Two genes, every child will get one.
Dr. Fine teaches that if a
patient has one gluten syndrome gene, there is a 50% chance that children will inherit the
gene. If a patient carries two genes, one gluten syndrome gene will pass to each
child, and both the patient's own parents carried at least one gene.
Quote: Having two copies of a gluten
sensitive [reactive] gene, means that each of your parents, and all of your children
(if you have them) will possess at least one copy of the gene. Two copies
also means there is an even stronger predisposition to gluten sensitivity
[reactivity] than having one gene and the resultant immunologic gluten sensitivity
[reactivity] may be
more severe. www.enterolab.com
 Close: Dr. Fine teaches that if a patient has one gene, there is a 50% chance...
Close: Dr. Fine teaches that if a patient has one gene, there is a 50% chance...
 If
gluten is presented to immune system with a gene, it will react.
 Other organs, tissues or functions may be damaged
INSTEAD of villi.
Other organs, tissues or functions may be damaged
INSTEAD of villi.
He believes other body
organs or tissues, or functions of the intestine and other body tissues may be
damaged INSTEAD of villi damage.
"In these non-celiac, gluten sensitive
[reactive] individuals, the brunt of the
immune reaction either affects the function of the intestine, causing
symptoms without structural damage, affects other tissues of the body
(and virtually all tissues have been affected in different individuals),
or both."
 Close: Other organs
Close: Other organs
 His stool
tests find elevated antibodies before blood
tests.
His stool
tests find elevated antibodies before blood
tests.
He claims his fecal tests
are more sensitive and identify antibodies in the gut before they cross into
the blood stream. He adjusts for expected antibodies in the gut.
Quotes: Up until recently it
was thought that nearly all patients with clinically important gluten
sensitivity [reactivity] had these antibodies detectable in blood. However, recent
studies, including my own, have shown that this is not true. In the early
phases of the reaction, or especially when the disease is of a more mild
variety, antigliadin and antiendomysial/antitissue transglutaminase
antibodies may be absent from blood.
Quote: "Knowing that the
immune reaction to gluten and it is not surprising to me that blood tests in
the early phase of gluten sensitivity [reactivity] are negative. This is because the
immunologic reaction to gluten begins and occurs inside the intestinal tract
and not in the blood per se."
 Close: He claims his fecal tests are more sensitive
Close: He claims his fecal tests are more sensitive
 Stool
test is usable for a time after a patient is gluten free. Stool
test is usable for a time after a patient is gluten free.
 Elevated antibodies are proof of an immune
response to gluten.
Elevated antibodies are proof of an immune
response to gluten.
He advises that elevated
antibodies are proof that there is an immune response to gluten grains, ie.
the body is fighting gluten and is gluten sensitive [reactive]. This
presumes a properly run test.
The immune reaction to
gluten is gluten [reactivity]. Testing for the presence of an antibody
produced against gluten is the diagnostic hallmark of gluten
[reactivity] or in other words the gluten syndrome.
A positive (antibody)
value of any degree means your immune system is reacting to dietary gluten
in the way the immune system reacts to an infection.
Some people may make more
antibodies than others so low numbers may not indicate a lesser reaction. (this
from Ken Fine)
 Close: Elevated antibodies are proof that there is an immune response
Close: Elevated antibodies are proof that there is an immune response
 Villi biopsy identifies villi damage and misses
damage elsewhere.
Villi biopsy identifies villi damage and misses
damage elsewhere.
He maintains that villi
biopsy only identifies those patients whose gluten induced damage
happens to include villi atrophy. Furthermore, Dr Fine believes in
some cases villi damage may be submicroscopic, ie, not be detectable under
a microscope. The major damage may be somewhere else in the body. Therefore he maintains that villi biopsy is an inappropriate, misleading
criteria for general gluten syndrome diagnosis. Biopsy may be needed if
there is suspicion of tumor or other gut disturbances.
Quote: The immune
reaction to gluten is gluten sensitivity [reactivity]. Testing for the presence of an
antibody produced against gluten is the diagnostic hallmark of gluten
sensitivity [reactivity] (for years in the blood, and now more sensitively detected in
stool with our testing). Although the immune reaction to gluten, i.e.,
gluten sensitivity [reactivity], is the cause of the villous atrophy of celiac sprue,
having these antibodies in stool, or even malabsorption, does not
necessarily mean you will have detectable villous atrophy in an intestinal
biopsy. But why does it matter, since it is known that a person can have
every last complication from gluten sensitivity [reactivity] and never have villous
atrophy? In other words, one can have gluten sensitivity [reactivity] damaging the
intestine on a sub-microscopic level destroying function, or damaging other
organs/tissues without having celiac sprue. Thus, there is no reason to
expose yourself to the risks, invasive nature, and expense of an intestinal
biopsy.
 Close: He maintains that villi biopsy
Close: He maintains that villi biopsy
 Dr. Fine's lab processes a high percentage of positives. Dr. Fine's lab processes a high percentage of positives.
Dr. Fine's lab processes a high
percentage of positives.
This is a major reason some
specialists question his
work. However many tests are submitted from patients who so strongly
question their standard test results that they pay out of pocket for his
tests, so his routine lab sampling is somewhat preselected. This
preselection phenomena does not apply to his controlled research projects
that in fact also return a high incidence of positives.
 Close: Dr. Fine's lab processes a high percentage of positives.
Close: Dr. Fine's lab processes a high percentage of positives.
Dr. Fine also optionally checks cross reactive milk,
soy, egg, and yeast.
 Close: B. Summary of Dr. Fine's announced conclusions
Close: B. Summary of Dr. Fine's announced conclusions
 C. Our family's scary experience -
C. Our family's scary experience -
Enterolab was the only accurate test.
C. Our family's testing experience
All 8 members of our
symptomatic family have a double copies of DQ 2 and/or 8, or 2 or 8
plus DQ 1 genes. We received negative full celiac panels
from a respected lab even though some actually had elevated AGA antibodies. My
husband received one positive and one negative tTG-IGA six months apart
while on a gluten containing diet. Later
our daughter Su, 22, a college
student, tried a 6 week gluten challenge after being off wheat
for 8.5 years, the last 6 months strictly gluten free. The challenge was
miserable, but her blood and biopsy tests at the end were "stone cold negative”
from a lab considered reliable. (Her Enterolab test was positive but we did
not know how much credibility to give that test.) Even
before she returned to a gluten free diet,
she began to crash into severe uncontrollable “black pit” depressions
which she termed "horrible" and they worsened a few days AFTER SHE
RETURNED TO A GLUTEN FREE DIET. This uncharacteristic instability continued for
3.5 months after she resumed a strict gluten free diet EXCEPT for
communion bread which she consumed once a week "since her blood and biopsy
tests were negative. She thinks she may have had a
breakdown and stated at the time that she might not ever be the same person.
Eventually upon our request, the church elders kindly
permitted us to provide a gluten free loaf for communion. Several weeks
after the loaf change, Su was able to describe to us how much better she
felt. She attributed this to the total elimination of gluten grains from
her diet. Over the next months, she continued to stabilize, paced her workload,
and
was very careful with her diet. However, four
months after the communion loaf change, she baked cookies with wheat flour
and, although she did not eat the cookies, she crashed again. Her
"black pit depression" reaction lasted about 2 weeks. Five months after the baking incident, she
had another “gluten grain mistake” and although she experienced severe
abdominal pain for days, she did not crash psychiatrically. Thankfully
she was able to graduate college with honors and degrees in both nursing and
Spanish.
Our family history on all 4 sides, genes, symptoms and good diet response
strongly indicate some type of reactivity to gluten grains. My husband’s
aunt is a diagnosed celiac. My husband, Su’s father, has been sick for 35 years.
Most of our children had symptoms as babies and children, and our sons also are redeveloping symptoms in their early twenties. Su appears to have
had the gluten syndrome from babyhood. She carries a double copy of the DQ 2 gene and the Enterolab test was positive.
Her standard blood tests and biopsy were negative. We now understand that the
blood panels
are very incomplete. Likely Su had other antibodies than the
ones they tested and neurological damage, not villi damage.
In our family's experience,
Su's body and Dr. Fine’s more sensitive tests told us the truth. We wish we'd trusted
that when an accredited lab finds antibodies they are real, they can hurt
us, and we should pay attention!! Validated science can catch up later
in this case and we hope that will be soon.
Update:
May 2007
Su works as a nurse and still
is doing well on a very very strict gluten and dairy free diet.
However, she has suffered an emergency appendectomy, back problems, a
fractured sternum, and for a short time a grumbling gall bladder. Her
emotional state is good, but still not quite as good as the six months she
was strictly gluten free just before her gluten challenge. The gluten
challenge was dangerous and unnecessary.
Her Enterolab test matched her
case. Likely a more detailed blood test such as the Immunosciences
Laboratories panel would have revealed antibodies that the shorter celiac
panel did not include.
Update January 2009
Su is doing very well.
She married a fine young man, also a nurse, last year and recently left her
hospital nursing job of over 3 years to do home health nursing. She is
very strict with her diet and her husband joins her in her diet in order to
support her. They go out of their way to make healthy lifestyle
choices.
 Close:
B. Our family's testing experience
Close:
B. Our family's testing experience
 Close: 2. Who is Dr. Ken Fine and what is the situation regarding his
Enterolab stool and gene tests?
Close: 2. Who is Dr. Ken Fine and what is the situation regarding his
Enterolab stool and gene tests?
 3. Why are the panels recommended by Immunosciences Labs so much more detailed when
other labs/celiac centers discontinued the antigliadin antibody
test?
3. Why are the panels recommended by Immunosciences Labs so much more detailed when
other labs/celiac centers discontinued the antigliadin antibody
test?
3. Why are the panels recommended by Immunosciences Labs so detailed when other
labs/celiac centers discontinued even the AGA antigliadin antibody test?
Tests not available at this
time. Watch home page of this website for further information.
Why have many specialists have discontinued the AGA test?
Many specialists discontinued the AGA test
because AGA antibodies often are elevated but there is no villi damage. Conservative doctors
insist that villi damage is the ONLY definitive marker of immune response to
gluten so they discount the presence of antibodies if there is no villi
damage (ie they believe the gliadin antigen is often false positive). They now test for elevated tTG instead, which
is usually directly connected to
villi damage.

Dr
Vojdani believes that properly run gliadin antibodies are accurate, reliably
prove immune response, and are dangerous.

Dr. Vojdani checks
IgA, IgG and
IgM antibodies.
Dr. Vojdani checks IgA, IgG,
and IgM
antibodies.
(Tests not available at this
time. Watch home page of this website for further information.)
This is like asking the Army, Navy and
Air Force to look for a criminal. They cover different areas.
IgA, IgG, and IgM are different subsystems of the immune system. To
"cover the bases" they may all need to be checked. Note:
Additionally IgE is the "allergy system". IgD is very poorly understood.
 Close: Dr. Vojdani checks IgA, IgG and IgM
Close: Dr. Vojdani checks IgA, IgG and IgM
 Dr. Vojdani checks more types of antibodies, including
gluten
itself.
Dr. Vojdani checks more types of antibodies, including
gluten
itself.
Dr.
Vojdani looks for
gluten antibodies, "gluteomorphins", wheat and AGA-tTG antibodies as well as antigliadin (AGA)
and tTG antibodies.
There are other glutenins for which there are no tests.
Question?
What are gluteomorphins and glutenins? I've never heard of them.
Answer:
Gluteomorphins, gliadin, and other glutenins are various pieces of
incompletely digested gluten.
*Gliadin
makes gluten stretchy. Glutenins let stretched gluten spring back to
original shape.
*(Cauvain,
Bread Making, 1-589)
Here is a quote from Dr. Aristo
Vojdani which discusses gluteomorphins:
"Gluteomorphins are very small
peptides of gluten the size of 8-80 amino acids. When gluten is broken
down by body enzymes to small peptides, some of these peptides bind to
receptors on the brain and immune system cells.
Since usually morphins bind to
these receptors, and gluten peptides also bind to these receptors, these
molecules are then called gluteomorphins, meaning molecules from gluten bind
to morphin receptors and act like morphins. That is why patients with
gluten sensitivity [reactivity] also have neurological involvements."
Aristo Vojdani, Ph.D, M. T.
8/23/2006
 Close :
Dr. Vojdani checks more types of antibodies
Close :
Dr. Vojdani checks more types of antibodies
 Patients do not all have the same antibodies.
Patients do not all have the same antibodies.
Patients do not
all have the same antibodies.
Some have gluteomorphins, gliadins, or gluten or wheat or one or several of
these. Dr. Vojdani recommends testing as many as necessary or possible
using IgA, IgG, and IgMs, looking for a possible positives.
Tests not available at this
time. Watch home page of this website for further information.
 Close: Patients do not all have the same antibodies.
Close: Patients do not all have the same antibodies.
 Glutamic Acid Decarboxylase
and gluten and diabetes Glutamic Acid Decarboxylase
and gluten and diabetes
-
Dr. Vojdani finds 65%
of celiacs have elevated Glutamic Acid Decarboxylase,
a substance that
indicates damage to the islet cells of the pancreas. Therefore he tests Glutamic Acid Decarboxylase in the Immunosciences
Celiac
Neuroautoimmune Panel and includes many other susceptible organ
damage/function tests.
Tests not available at this time.
Watch home page of this website for further information.
 Close: Glutamic Acid Decarboxylase
Close: Glutamic Acid Decarboxylase
 Cellular (Molecular) Mimicry - Predictive Antibodies
Cellular (Molecular) Mimicry - Predictive Antibodies
 Immunosciences Labs and other labs test for cross reactive foods that
look similar to gluten, such as corn, egg, milk, yeast and soy.
Immunosciences Labs and other labs test for cross reactive foods that
look similar to gluten, such as corn, egg, milk, yeast and soy.
It is
believed toxins stress and infections may create a
gut wall that is too permeable or leaky. This may cause the
body to create antibodies to other incompletely digested foods and substances
that slip past the gut wall . Those foods
and substances may keep the
immune system reacting even when some of the offenders like gluten or milk are
removed from the diet. Therefore some of these other substances may
also be removed in order to calm the immune system's hyperreactions.
Other strategies may be needed to accomplish this and professionals may be needed to determine how to
heal the gut and calm down the immune system.
 Close link: Immunosciences Labs and other labs test
other foods
Close link: Immunosciences Labs and other labs test
other foods
 Close
link: Why are the Immunosciences Labs testing panels more detailed. Close
link: Why are the Immunosciences Labs testing panels more detailed.
 4. I've never heard of the ALCAT and
ELISA/ACT Biotechnologies tests. What do they test? How are they different from
each other and other tests?
4. I've never heard of the ALCAT and
ELISA/ACT Biotechnologies tests. What do they test? How are they different from
each other and other tests?
The ALCAT test is a separate
type of test compared to other tests on this page. In this method,
white blood cells are exposed to various foods and other substances such
as additives separately and the reaction of the cells is
observed. This lab includes gliadin
and gluten testing in their panels.
A simple analogy is that
traditional tests of IgM, IgG and IgA antibodies are similar to
"calling up" the Army, Navy and Air Force to find a criminal. (See "Stories
to Help Us Understand" above). The ALCAT method is likened to
"calling in" the National Guard. It's another way to look for adverse response in the immune system.
Opinions vary regarding the reliability of this test.
More information about
this method is found at
www.alcat.com
A
prescription is not mandatory and arrangements can be made for a
nurse/phlebotomist to perform the blood draw at home. Post test
counsel is included in the test package. Note: this test is controversial.
Some professionals believe it mainly reacts to foods eaten frequently.
Some patients say it helped them pinpoint their problem substances.
-
The ELISA/ACT Biotechnologies is a
similar test to ALCATin that it tests specific white blood cells called
lymphocytes for a specific reaction to gluten related items.
Lymphocytes are the cells inside which antibodies are made. They
burst and spill the antibodies into the blood stream. If the grain
or gluten incites a reaction the antibodies produced inside the lymphocyte
cause it to swell and a halo forms around the cell prior to bursting.
The swelling and halo indicate a positive test. This test
requires a serving of gluten or grain tested within the past 6 months. It
is offered in panels of multiple foods including gluten and non gluten
grains, molds, chemicals, food additives, etc. Gliadin, gluten, wheat, and
a number of other gluten and gluten substitute grains are included in the
panels.
 Close link: 4. I've never heard of the ALCAT test. What does it test and how is it different from other tests?
Close link: 4. I've never heard of the ALCAT test. What does it test and how is it different from other tests?
5. Help!! No one
knows how to read my gene test!!
Gene chart coming
 6. What about saliva tests? 6. What about saliva tests?
Saliva tests were previously used more commonly in Europe than the United
States. More research is available now, and they used more frequently
as initial screeners by some practitioners. It is believed that
antibodies also may hang out in the saliva as early markers of immune
reaction at least in some cases. Major celiac (villi focused)
specialists still do not usually use them.
A new
home saliva test
screener
is coming soon that checks 4 antibodies, Gliadin IgA and IgG, and tTG-IgA and IgG. The new tests is claimed to be
96% sensitive if the patient has those antibodies present in the saliva.
It's advantage is that it is a quick and quick and inexpensive first step test.
If it is negative, patients can go on to other more comprehensive antibody tests, or use
a progressive test (proposed) with this saliva test as a first step in the
progression.
 Close: What about saliva tests?
Close: What about saliva tests?
 7. What about finger stick blood tests that check for IgG antibodies? 7. What about finger stick blood tests that check for IgG antibodies?
7. What about finger stick blood tests that check for IgG
antibodies?
These tests usually check
either of two
very common antibody types, IgA or IgG.
Optimum Health Resource Laboratories offer these tests.
However, in the case of their celiac tests they run some IgA and IgM tests.
Their 96-food panel tests both gliadin (wheat) and gluten.
Recent research on this type of testing is posted on their website.
These tests check a lot of foods in just one or sometimes 2 places in the
immune system. As with all antibody panels, there are more markers to
test so a positive can be helpful a negative is inconclusive.
 Close: 7. What about finger stick blood tests that check for IgG antibodies?
Close: 7. What about finger stick blood tests that check for IgG antibodies?
 8. What about Electroaccupuncture according to Voll? 8. What about Electroaccupuncture according to Voll?
8. What about
electroaccupuncture
according to Voll?
This alternative energy
based method has gained popularity in recent years. The machines
work by measuring the vibrational signatures of various tissues and
substances in the body. The machines and methods have been refined
through about 8 stages in the past approximately 20 years. Some
patients try it for diagnosis of a reactivity, for possible additional
information, or to compare with other tests or their body's own messages.
It's accuracy or sensitivity is debated depending on the professional
questioned.
Networking with experienced patients
may be helpful.
 Close: What about Electroaccupuncture according to Voll
Close: What about Electroaccupuncture according to Voll
|